Epilepsy is a chronic neurological disorder affecting millions worldwide.
It’s characterized by recurrent seizures caused by abnormal electrical activity in the brain.
While anti-epileptic drugs (AEDs) are the cornerstone of treatment and control seizures in most patients, a significant percentage of them do not respond adequately to drug therapies.
This leaves them vulnerable to recurrent and debilitating seizures that significantly affect their daily quality of life, their ability to work, and even their personal safety.
In the face of this challenge, surgical interventions have emerged as a promising treatment option, among them “epilepsy battery surgery,” or what is medically known as Vagus Nerve Stimulation (VNS).
This technique, which relies on implanting a device to modulate the brain’s electrical activity, offers a glimmer of hope for patients who have exhausted traditional treatment options.
It aims to reduce the frequency and severity of seizures, thereby significantly improving their quality of life.
Doctors, in centers like Liva Hospital in Turkey, conduct a thorough evaluation of potential VNS candidates, including a complete medical history review and electroencephalogram (EEG) to assess cognitive functions.

Epilepsy and the Role of Vagus Nerve Stimulation
To delve into the true indications for VNS surgery, it’s essential first to understand the concept of “refractory epilepsy.”
Refractory epilepsy is defined as the inability to achieve sustained seizure control using adequate doses of at least two appropriately chosen and well-tolerated anti-epileptic drugs, either as monotherapy or adjunctive therapy.
This means the patient has tried multiple treatment approaches without success, and their life is still severely affected by seizures. In such cases, seeking alternatives becomes imperative.
Here, Vagus Nerve Stimulation (VNS) comes into play. The vagus nerve is the longest cranial nerve, extending from the brainstem to many organs in the neck, chest, and abdomen.
This nerve plays a vital role in regulating many involuntary bodily functions, including heart rate, breathing, and digestion, and has extensive connections with the brain.
VNS technology exploits these connections by sending regular electrical impulses to the brain via the vagus nerve.
These impulses are believed to modulate the abnormal electrical activity in the brain that causes seizures, leading to a reduction in their frequency and severity, and sometimes even completely stopping them in some cases.
Unfortunately, VNS is not a cure, but it is a palliative treatment aimed at improving quality of life and seizure control.
True Indications for VNS Surgery
The decision to implant a Vagus Nerve Stimulation (VNS) device is a significant medical decision made only after a comprehensive and thorough evaluation by a multidisciplinary medical team.
The true indications for performing this procedure revolve around treating refractory epilepsy, but within the framework of specific criteria to ensure the best possible outcomes for the patient:
- Refractory Epilepsy: As mentioned, this is the primary criterion. The patient must have tried at least two appropriate anti-epileptic drugs at sufficient therapeutic doses and tolerated them well, without achieving seizure control.
- Partial or Generalized Seizures Unresponsive to Medication: VNS is considered particularly effective in cases of partial epilepsy (which originates in a specific area of the brain), but it may also be used in some forms of generalized epilepsy.
- Patient Ineligibility for Resective Epilepsy Surgery: In some cases, epilepsy is caused by a specific area that can be surgically removed (resective epilepsy surgery), which can achieve complete cure.
However, if the seizure-causing area is located in a sensitive region of the brain that cannot be safely resected (such as language or motor areas), or if the epilepsy originates from multiple foci, VNS becomes a safe and effective alternative. - Epilepsy Patients with Severe Medication Side Effects: Even if medications can partially control seizures, severe side effects affecting the patient’s quality of life may make VNS an acceptable option.
- Children and Adolescents: VNS is an approved treatment option for children over 4 years old who suffer from medically refractory epilepsy.
- Realistic Expectations: The patient and their family must be aware that VNS is not a cure, and the primary goal is to reduce the frequency and severity of seizures, not to eliminate them completely in most cases.
Surgical Procedure for VNS Implantation
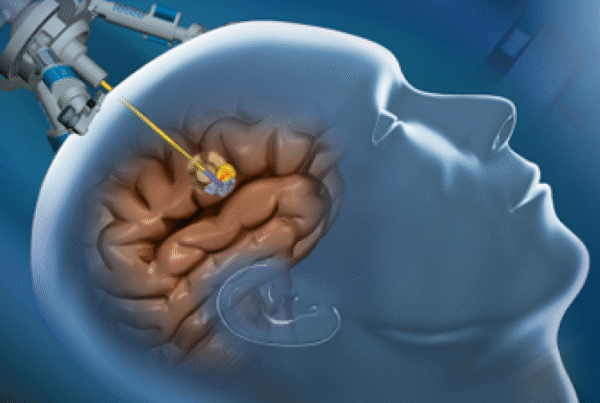
The procedure for implanting a Vagus Nerve Stimulation (VNS) device is relatively simple compared to other open brain surgeries and is usually performed under general anesthesia.
The operation typically takes between one to two hours and involves two main steps:
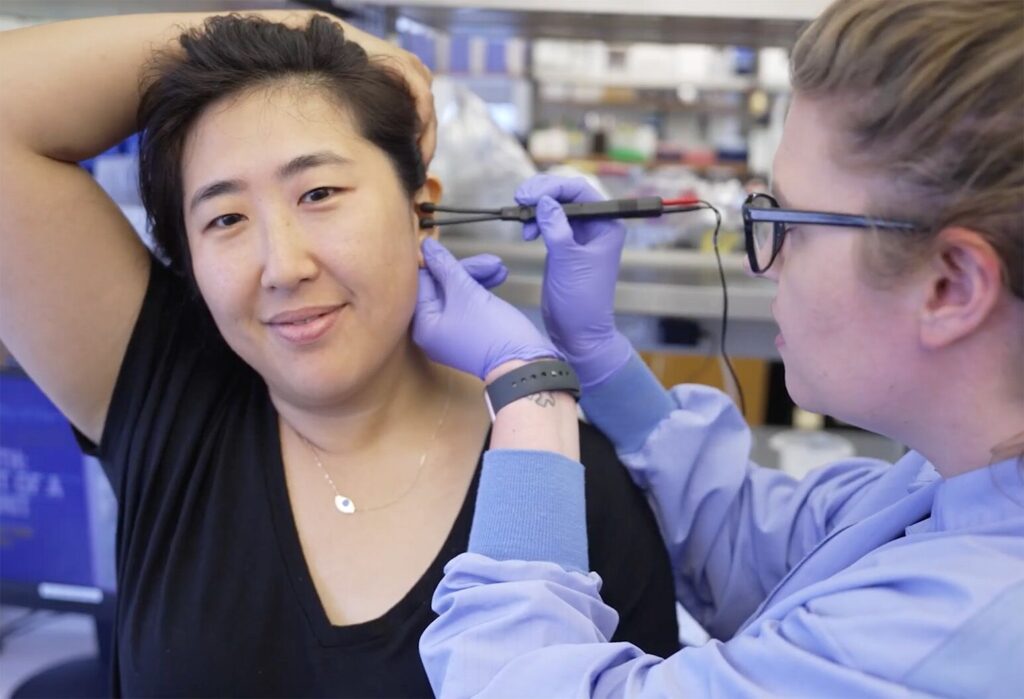
- Implanting the Electrode on the Vagus Nerve: The surgeon makes a small incision on the left side of the neck (usually because the left vagus nerve does not play a major role in heart functions, reducing the risk of cardiac side effects).
The vagus nerve is precisely located, and a thin electrode is then wrapped around it. This electrode is designed to be in direct contact with the nerve without damaging it. - Implanting the Pulse Generator (Battery): The surgeon makes another small incision on the left side of the chest, usually under the collarbone or in the armpit area. A small pocket is created under the skin where the pulse generator (battery) is placed.
The wires coming from the electrode implanted around the vagus nerve are connected to the pulse generator under the skin, and all wires are hidden under the skin.
After the implantation is complete, the surgeon tests the device to ensure it is working correctly. The surgical incisions are closed, and the patient can usually return home the same day or the next.
Post-Surgery and Device Programming
The VNS device does not begin to operate at full capacity immediately after surgery. The post-surgery phase, specifically device programming, is a vital part of the treatment.
The device is usually activated about two to four weeks after surgery to allow the wounds to heal. This is done in the neurologist’s office using a special programming device placed over the implanted battery.
- Initial and Gradual Programming: The neurologist programs the device to deliver electrical impulses to the vagus nerve at a specific frequency, duration, and intensity.
Programming usually starts with low settings and gradually increases over weeks or months. This gradual approach helps the brain adapt to the stimulation and reduces potential side effects. - Regular Follow-up: The VNS process requires regular follow-up with the neurologist to adjust settings based on the patient’s seizure response and any side effects.
The goal is to find the optimal setting that reduces seizures with the fewest side effects. - Magnet Use: The patient is given a magnet that can be used to activate the device when they feel a seizure coming on (aura), which may help stop the seizure or reduce its severity.
It can also be used to temporarily increase stimulation during periods of increased seizure frequency.
Comprehensive Cost of VNS Surgery
Cost is an important factor to consider when deciding on VNS surgery. The comprehensive cost varies significantly based on several factors, including the country where the procedure is performed, the hospital, the surgeon’s experience, and the type of device implanted.
- Cost of the Device Itself: The Vagus Nerve Stimulation device itself is the most expensive component of the procedure. Device prices vary depending on the manufacturer and features (such as whether they are rechargeable or not).
- Hospital Fees: These fees include the use of the operating room, hospital stay (if required), and medical equipment.
- Surgeon and Anesthesiologist Fees: These fees vary based on the surgeon’s experience and reputation, as well as the complexity of the case.
- Pre-Surgery Tests: These tests include magnetic resonance imaging (MRI), electroencephalogram (EEG), and specialized medical consultations.
- Programming and Follow-up Sessions: These sessions are essential after surgery and include clinic fees and doctor’s fees.
- Battery Replacement Cost: In the case of non-rechargeable batteries, they will need to be surgically replaced after several years, which adds an additional cost in the future.
Generally, the total cost of VNS implantation surgery in developed countries like the United States or Western Europe can range from $25,000 to $50,000 USD or more, depending on the factors mentioned above.
In contrast, countries like Turkey offer high-quality treatment options at competitive prices.
For example, at Liva Hospital in Turkey, the total cost of VNS implantation can be significantly lower, while maintaining international quality standards, making it an attractive destination for patients seeking effective treatment at a reasonable cost.
Potential Side Effects and Treatment Effectiveness
Like any medical intervention, Vagus Nerve Stimulation can be accompanied by some side effects, although they are usually mild and temporary.
- Common Side Effects: These include hoarseness, coughing, sore throat, shortness of breath, or a change in voice during stimulation. These side effects are often related to the stimulation settings and can be reduced by adjusting them.
- Less Common Side Effects: These may include infection at the incision site, device or wire problems, or pain at the implant site.
- Rare Surgical Risks: Such as bleeding or damage to surrounding nerves.
As for effectiveness, studies show that VNS provides significant improvement in seizure control for the majority of patients. This procedure is not intended to completely eliminate seizures in all cases, but it demonstrates:
- Reduction in Seizure Frequency: A 50% or greater reduction in seizure frequency is observed in 40-50% of patients.
- Reduction in Seizure Severity: Even if seizure frequency does not decrease significantly, their severity may decrease, making them less impactful on the patient’s life.
- Improvement in Quality of Life: Improved seizure control leads to an overall improvement in quality of life, including increased independence, improved mood, and reduced seizure-related injuries.
Conclusion
Vagus Nerve Stimulation (VNS) has revolutionized the approach to treating refractory epilepsy, offering real hope to patients who have not responded to traditional drug therapies.
Thanks to advancements in surgical techniques and programming settings, this procedure has become safer and more effective in reducing the frequency and severity of seizures.
Although cost is an important consideration, the availability of high-quality treatment options at competitive prices in international centers like Liva Hospital in Turkey makes this therapy accessible to a larger number of patients worldwide.
Frequently Asked Questions
Is the Vagus Nerve Stimulation (VNS) device a permanent cure for epilepsy?
No, the VNS device is not a cure for epilepsy. It is a palliative treatment aimed at reducing the frequency and severity of seizures. The disease remains present, and in most cases, the patient needs to continue taking anti-epileptic drugs.
How long does it take to see improvement after VNS surgery?
Improvement is usually not immediate. The programming process begins a few weeks after surgery, and settings are adjusted gradually. It may take several months or even a year to observe the maximum improvement in seizure control.
Can I remove the VNS device if it doesn’t work or if I want to?
Yes, the VNS device can be surgically removed if it is not effective or if the patient decides to remove it for any reason. However, the removal process is another surgical procedure.
Will the VNS device affect daily activities like sports or using mobile phones?
Generally, the VNS device does not affect most daily activities. Patients can engage in sports and normal activities. Some powerful electrical equipment or medical devices (such as MRI) may require special precautions or may be prohibited in some cases.
What is the minimum age for VNS device implantation?
The Vagus Nerve Stimulation (VNS) device is approved for use in children over 4 years old who suffer from medically refractory epilepsy and have not responded to medications.
What happens when the device’s battery runs out?
When the device’s battery (pulse generator) runs out, it must be surgically replaced. For non-rechargeable batteries, this typically occurs every 3 to 5 years.