The kidneys are vital organs in the human body, playing an indispensable role in filtering waste and toxins from the blood, regulating blood pressure, and producing essential hormones.
However, when the kidneys completely fail to perform their functions, known as End-Stage Renal Disease (ESRD), it becomes life-threatening.
At this stage, dialysis becomes a crucial necessity to sustain the patient’s life.
Nevertheless, dialysis is not a cure; it is a temporary solution that does not prevent the continuous deterioration in quality of life associated with kidney failure.
Here, kidney transplantation emerges as a radical and life-changing treatment option.
Kidney transplantation offers patients the opportunity to restore normal kidney function, eliminate the constraints of dialysis, and significantly improve their quality of life.
We find in numerous success stories, such as those recorded at Liva Hospital in Turkey, the effectiveness of this operation compared to dialysis, with superior results in terms of quality of life and survival rates.
Chronic Kidney Failure
To understand the importance of kidney transplantation, it is essential to realize the severity and impact of chronic kidney failure on a patient’s life.
Chronic kidney disease develops gradually over years, and symptoms often do not appear until the damage reaches a very advanced stage.
When the kidneys lose their ability to filter blood effectively (usually when kidney function is less than 15% of normal), toxins accumulate in the body, leading to a wide range of health problems that affect all body systems.
This stage is known as End-Stage Renal Disease (ESRD), at which point renal replacement therapy becomes a crucial necessity.
Types of Kidney Transplantation: Deceased Donor vs. Living Donor?
Kidney transplantation offers patients two main options for obtaining a new kidney, both of which have specific advantages and challenges: deceased donor kidney transplant and living donor kidney transplant.
Both methods are safe and effective, and the most suitable method is chosen based on organ availability, the patient’s condition, and medical recommendations.
Leading centers in the region, such as Liva Hospital in Turkey, offer extensive experience in both types of kidney transplant operations, with a focus on the safety of both donor and recipient.
Understanding these options is crucial for the patient and their family to make the most appropriate decision.
Deceased Donor Kidney Transplant
This is the most common option for kidney transplantation in many countries worldwide.
Kidneys are obtained from a recently deceased person (usually due to severe brain injury or cardiac arrest), after family consent and ensuring that the kidneys are healthy and free of disease.
After retrieval, the kidneys are examined and prepared for transplantation to the most compatible patient on a national or regional waiting list.
- Advantages:
- Does not require surgery on another living person, removing the risks associated with living donation.
- The patient can benefit from an organ that has been thoroughly examined before transplantation.
- Challenges:
- Organ Scarcity: The lack of available organs is the biggest challenge. This leads to very long waiting lists, which can extend for many years, and some patients may die while waiting for a suitable organ.
- Unpredictable Timing: The time of organ availability cannot be predicted, requiring the patient to be ready for surgery at any moment upon receiving the call.
Living Donor Kidney Transplant (LDKT)
This option is preferred and safer in many specialized centers due to its numerous advantages.
In this type, a living person (usually a family member, friend, or even an anonymous donor) donates one of their kidneys to the recipient patient. The donor’s remaining kidney fully compensates after adaptation.
- Living Donation Process: The potential donor undergoes a very comprehensive and intensive medical and psychological evaluation to ensure their complete health, that they have no diseases that increase the risks of donation, and that they are donating voluntarily.
Blood type and tissue compatibility (HLA matching) with the recipient are performed. Kidney removal from the donor is usually done using laparoscopy, a minimally invasive surgical technique that reduces pain and recovery time for the donor. - Key Advantages of Living Donor Kidney Transplant:
- Avoid Long Waiting Lists: The patient can receive a kidney much faster, which reduces their suffering period on dialysis and improves outcomes.
- Better Long-Term Outcomes: Studies show that living donor kidneys typically last longer and function better compared to deceased donor kidneys.
- Optimal Organ Quality: Living donor kidneys are often in excellent health due to the comprehensive donor screening.
- Planned Procedure: The surgery date can be planned in advance, allowing for better preparation for both recipient and donor.
- Paired Kidney Exchange Programs: In cases where a person wishes to donate to a recipient but there is no blood type or tissue match, they can enter a paired kidney exchange program.
This involves swapping kidneys between incompatible pairs to create chains of compatible transplants, increasing the chances for patients to receive kidneys.
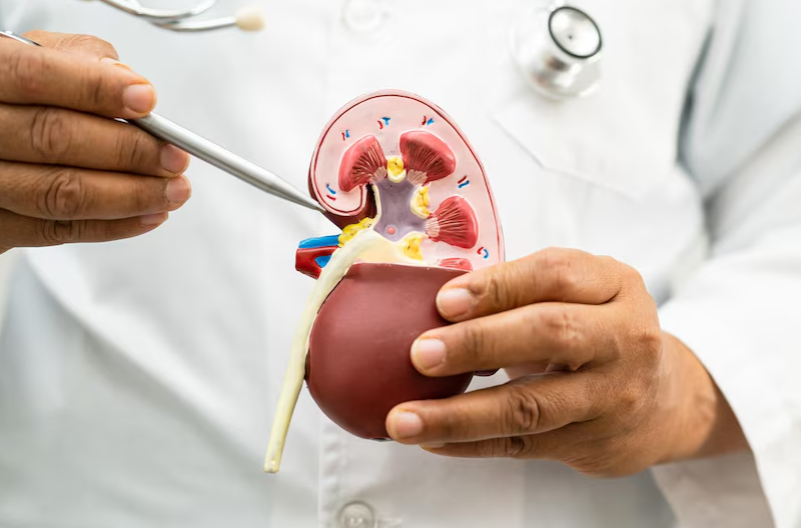
Steps of Kidney Transplantation
Kidney transplantation is a major surgical procedure but is routine in specialized transplant centers. The operation usually takes between 2 to 4 hours.
Pre-Surgical Preparation
- The recipient and donor (in the case of living donation) are prepared for surgery. This includes fasting, prophylactic antibiotic administration, and preparing the surgical area.
- Intravenous lines and catheters are inserted to monitor vital signs and fluids.
- The patient is placed under general anesthesia.
Kidney Removal from the Donor (Donor Nephrectomy) – in Living Donation Cases
- This step is usually performed before or concurrently with the start of the recipient’s surgery.
- This operation is often performed using laparoscopic surgery, a minimally invasive technique that involves making several small incisions in the abdomen to insert a camera and surgical instruments.
The kidney is removed through one of these incisions or through a slightly larger incision (Minimally Invasive Open).
- Laparoscopic surgery is less painful and has a faster recovery time for the donor compared to traditional open surgery.
- After removal, the kidney is cooled with a special solution to protect it during transport to the other operating room.
Recipient Preparation and Kidney Implantation (Recipient Transplant)
- A surgical incision is made in the lower part of one side of the recipient’s abdomen.
The recipient’s diseased kidneys are usually not removed unless they cause problems (such as infection or severe high blood pressure). - The new kidney is placed in the pelvis (usually in the lower right side), outside the peritoneal cavity (outside the intestines), which facilitates future access if needed.
- The new kidney is then connected to the recipient’s blood vessels:
- Renal Artery from the donor kidney is connected to the recipient’s internal or external iliac artery.
- Renal Vein from the donor kidney is connected to the recipient’s external iliac vein.
- Ureter Connection: The ureter from the new kidney is connected to the recipient’s bladder. In some cases, a temporary stent is placed in the ureter to aid urine flow and prevent strictures.
- Confirming Blood Flow: After connecting the vessels, good blood flow to the new kidney is confirmed, and it usually starts producing urine immediately.
Recovery and Closure
- After ensuring the stability of the transplanted kidney, the surgical incisions are carefully closed.
- The patient is transferred to the Intensive Care Unit (ICU) for close monitoring.
These steps demonstrate the complexity and specialization required in kidney transplant surgery, which is underscored by the high level of care in advanced centers such as Liva Hospital in Turkey, which adheres to the latest surgical protocols to ensure the safety and success of the operation.
Long-Term Care
- Lifelong Adherence to Immunosuppressive Medications: This is the biggest challenge. The patient must take these medications precisely at the specified times and doses, and not miss any dose. Non-adherence can lead to kidney rejection.
- Side Effects of Immunosuppressive Medications: These medications can cause numerous side effects that require careful management, such as:
- Increased risk of infection: Due to immune system suppression, patients are more susceptible to bacterial, viral (e.g., CMV, EBV), and fungal infections.
- Kidney problems (in original kidneys): Some immunosuppressive medications may affect the function of the remaining kidneys.
- High blood pressure, diabetes, and high cholesterol: May require management of these conditions.
- Osteoporosis: Due to corticosteroid use.
- Increased risk of certain types of cancer: Such as skin cancers and some lymphomas, due to immunosuppression.
- Gastrointestinal or neurological problems: Such as nausea, tremors.
- Side Effects of Immunosuppressive Medications: These medications can cause numerous side effects that require careful management, such as:
- Organ Rejection: Despite immunosuppressive medications, there is still a risk of kidney rejection.
Rejection can be acute (occurring in the first weeks or months) or chronic (occurring after years). Acute rejection requires intensive treatment to save the kidney. - Regular Medical Follow-up: Transplant patients must undergo regular laboratory tests and frequent visits to the transplant clinic to monitor kidney function, immunosuppressive drug levels, and detect any complications early.
- Healthy Lifestyle: Patients are encouraged to follow a healthy diet, engage in moderate physical activity, and maintain a healthy weight. Alcohol and smoking should be completely avoided.
- Psychological Support: Psychological and emotional support is very important for patients and their families to cope with the physical and psychological challenges associated with transplantation.
Expected Outcomes After Kidney Transplantation
Kidney transplantation is one of the most successful and impactful medical interventions on the quality of life for patients with chronic kidney failure.
Despite the challenges and risks, the benefits often far outweigh the limitations of dialysis.
Survival Rates
Survival rates have improved significantly over decades.
- For deceased donor kidneys: Graft survival rates are about 90% after one year and 70-75% after 5 years. Patient survival rates are slightly higher.
- For living donor kidneys: Living donor kidneys show better results, with graft survival rates of about 95% after one year and 80-85% after 5 years.
- The lifespan of a transplanted kidney varies, with some kidneys lasting for many decades. If the transplanted kidney fails, the patient can return to dialysis or consider another transplant.
Improved Quality of Life
- Freedom from Dialysis: This is the most obvious benefit. Patients are freed from strict dialysis schedules, giving them greater freedom to travel, work, and engage in social activities.
- Improved General Health: A significant improvement in energy levels, appetite, better sleep, and a reduction in anemia are observed. Cardiovascular functions improve.
- Improved Quality of Life: In general, patients after kidney transplantation enjoy a much better quality of life compared to the period they were on dialysis. They can return to work, study, exercise, and raise families.
- Reduced Dietary and Fluid Restrictions: Although a healthy diet is still needed, the strict food and fluid restrictions imposed during dialysis are significantly eased.
Living with a Transplanted Kidney
- Adherence is Key: To ensure the best results, patients must strictly adhere to immunosuppressive medications, regular follow-up appointments, and a healthy lifestyle.
- Self-Awareness: Patients should be aware of the signs of kidney rejection or infection and report any changes to their healthcare team immediately.
- Continuous Support: Patients benefit greatly from continuous support from the healthcare team, family, and support groups.
Kidney transplantation is a long and comprehensive journey, but it offers hope for a healthy and full life for people with kidney failure. It is an investment in the future that is well worth every effort.
Conclusion
Kidney transplantation is considered one of the modern medical miracles that has changed the lives of millions around the world, offering a glimmer of hope and a new life for patients who were suffering from the burden of chronic kidney failure.
The available options, whether from a deceased or living donor, provide effective solutions for this intractable condition, with a strong emphasis on donor and recipient safety at every stage of the process.
From the complex evaluations preceding surgery, through the precise surgical techniques for kidney transplantation, to intensive post-surgical care and lifelong management of immunosuppressive medications, this journey is a test of human determination and medical dedication.
Thanks to continuous progress in this field and the availability of world-class medical centers such as Liva Hospital in Turkey, kidney failure patients can restore kidney function, be freed from the constraints of dialysis, and enjoy a significantly improved quality of life.
Frequently Asked Questions
How long does kidney transplant surgery take?
The surgery itself usually takes between 2 to 4 hours. However, the entire process from anesthesia to recovery may take several additional hours.
How long does a transplanted kidney last?
The lifespan of a transplanted kidney varies. On average, kidneys from deceased donors last about 10-12 years, while kidneys from living donors last about 15-20 years or more. Many kidneys continue to function much longer.
Can I stop dialysis immediately after transplantation?
In most cases, the new kidney begins to function immediately after surgery, and the patient can stop dialysis. However, some patients may need a few additional dialysis sessions in the first few days after surgery until the new kidney begins to function at full capacity.
What are the main side effects of immunosuppressive medications?
Common side effects include an increased risk of infection, high blood pressure, diabetes, high cholesterol, osteoporosis, and an increased risk of certain types of cancer. These side effects should be discussed with your healthcare team.
Can a pregnant woman undergo a kidney transplant or become pregnant after transplantation?
Transplantation is rarely performed during pregnancy except in extreme emergencies. However, women who have undergone a kidney transplant can become pregnant and give birth to healthy babies.
What happens if the transplanted kidney fails?
If the transplanted kidney fails, the patient can return to dialysis again, or they can enter the waiting list for another kidney transplant if they are eligible.


