Cancer has long been one of the most challenging and complex diseases, with researchers and doctors striving to find more effective and less harmful treatments.
Amidst this quest, immunotherapy has emerged as a revolutionary innovation, redefining the concept of cancer combat.
Instead of directly targeting cancer cells with chemicals or radiation, immunotherapy harnesses the power of the body’s innate immune system, training it to recognize and eliminate cancer cells.
This innovative approach represents a paradigm shift in cancer treatment, opening new horizons for patients who previously had limited treatment options.
In this context, Liva Hospital in Turkey has emerged as an advanced model that applies the latest immunotherapy techniques and provides comprehensive care to international patients.
The Complex Link between the Immune System and Cancer
To understand how immunotherapy works, it’s essential to first grasp the complex relationship between the immune system and cancer cells.
The immune system is a natural and astonishing defense system, consisting of an intricate network of cells, organs, and proteins that work in coordination to protect the body from pathogens like bacteria and viruses.
Under normal circumstances, the immune system can identify and eliminate cancer cells that arise in the body before they multiply and form tumors.
However, cancer cells possess a unique ability to “evade” the immune system’s response.
They can do this by producing proteins that suppress immune cells, by hiding their surface markers that allow immune cells to recognize them.
This immune evasion is what allows cancer to grow and spread. Immunotherapy understands and targets these mechanisms, aiming to “awaken” and reactivate the immune system so it can launch an effective attack against cancer cells.
Mechanisms of Action of Immunotherapy
The effectiveness of immunotherapy is based on a variety of mechanisms aimed at enhancing or unleashing the immune system’s response against cancer.
One of the most prominent of these mechanisms is the use of immune checkpoint inhibitors.
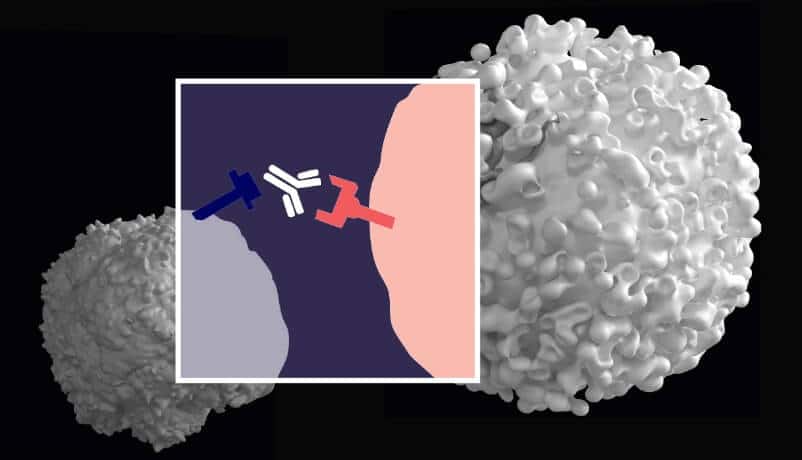
Checkpoints are molecules located on the surface of immune cells, such as T-cells, or cancer cells, and act as natural “brakes” to prevent overactivity of the immune system that could harm healthy tissues.
However, cancer cells exploit these checkpoints to avoid detection and destruction by the immune system.
Checkpoint inhibitors (such as PD-1/PD-L1 and CTLA-4 inhibitors) work by blocking these inhibitory signals, thereby freeing T-cells and allowing them to recognize and attack cancer cells more effectively.
Another important mechanism is CAR T-cell therapy, where T-cells are withdrawn from the patient’s blood, genetically modified in the laboratory to produce surface receptors (CARs) to recognize specific proteins on the surface of cancer cells.
This type of therapy shows promising results in some types of blood cancers. There are also therapeutic cancer vaccines, which aim to stimulate an immune response against specific proteins expressed by cancer cells.
Additionally, immune-stimulating agents such as interleukins or interferons are used to enhance general immune system activity.
Types and Clinical Applications of Immunotherapy
Advances in understanding the immune system have led to the development of multiple types of immunotherapies, each targeting different aspects of the interaction between cancer and the immune system.
The most prominent of these types are Immune Checkpoint Inhibitors, which include drugs such as Pembrolizumab (Keytruda), Nivolumab (Opdivo), Ipilimumab (Yervoy), and Atezolizumab (Tecentriq).
These drugs are now widely used in the treatment of many types of cancer, including melanoma (skin cancer), non-small cell lung cancer, kidney cancer, bladder cancer, colorectal cancer, and many more.
These drugs have brought about a true revolution in the treatment of these cancers, showing long-lasting responses in some patients.
Another important type is CAR T-cell therapy, which has been approved for the treatment of certain types of leukemia and lymphoma that have not responded to other treatments.
Despite its complexity and high cost, it offers impressive results in selected cases. There are also therapeutic cancer vaccines, such as the prostate cancer vaccine (Sipuleucel-T), which stimulates the immune system to fight cancer cells.
Additionally, interferons and interleukins, which are natural proteins produced by the body, are used to enhance the immune response in some types of cancer, such as kidney cancer and melanoma.
The expanding use of these treatments reflects the effectiveness of this approach and its ability to change the course of the disease for many patients.
For example, in specialized centers like Liva Hospital in Turkey, the latest internationally approved immunotherapies are provided, ensuring patients have access to the most advanced and best treatment options available.
Potential Benefits of Immunotherapy
Immunotherapy offers several potential benefits that distinguish it from traditional cancer treatments, making it a valuable addition to the arsenal of therapeutic approaches.
One of the most prominent benefits is the possibility of achieving long-lasting therapeutic responses and even cure in some cases.
Unlike chemotherapy and radiation, which target rapidly dividing cells and whose effectiveness may diminish over time as cancer cells develop resistance, immunotherapy teaches the immune system how to recognize and continuously eliminate cancer cells.
This means that some patients may achieve long periods of disease control, even after discontinuing treatment.
Another important benefit is the improved quality of life for patients.
While chemotherapy can cause severe systemic side effects such as nausea, hair loss, and bone marrow suppression, the side effects of immunotherapy are often different and may be less burdensome for some patients, although they can sometimes be serious.
Additionally, immunotherapy can be effective in treating types of cancer that do not respond to traditional treatments, offering a treatment option for patients who previously had little hope.
It can also be used in combination with other treatments, such as chemotherapy or radiation, to enhance their effectiveness and provide a more comprehensive treatment approach.
These combined benefits make immunotherapy a promising and exciting option in the fight against cancer.
Side Effects of Immunotherapy
Despite its significant benefits, immunotherapy is not without side effects.
Since immunotherapy works by activating the immune system, side effects are often the result of an overactive immune system attacking healthy tissues in the body, referred to as Immune-Related Adverse Events (irAEs).
These side effects can affect any organ in the body, and their severity and type vary from patient to patient.
Among the most common side effects are dermatitis (rash and itching), colitis (diarrhea and abdominal pain), thyroiditis (changes in thyroid hormone levels), hepatitis (changes in liver function), and hypophysitis (inflammation of the pituitary gland).
In rare cases, more serious side effects can occur, such as myocarditis (inflammation of the heart muscle) or pneumonitis (inflammation of the lungs).
It is essential for patients to recognize and report these side effects immediately to the medical team, as early detection and effective management are crucial for controlling them.
Management of these side effects often involves administering immunosuppressive drugs, such as corticosteroids, to calm the immune system and prevent further damage to healthy tissues.
In some severe cases, temporary or permanent discontinuation of immunotherapy may be required.
Dealing with these side effects requires a multidisciplinary medical team specializing in immunotherapy.
Challenges and Limitations in Immunotherapy
Despite the remarkable successes achieved by immunotherapy, it still faces some challenges and limitations that warrant further research and development.
The biggest challenge is that not all patients respond to immunotherapy. While some patients achieve amazing and long-lasting responses, others do not benefit at all, and there is a critical need for biomarkers that can better predict who will respond to treatment.
This would help avoid giving ineffective treatment to some patients, saving them time, side effects, and costs.
Another challenge is the high cost of immunotherapy, making it inaccessible to everyone worldwide and placing a significant burden on healthcare systems.
Also, immune-related side effects, although manageable, can be severe and sometimes life-threatening, requiring careful monitoring and clinical expertise.
Additionally, resistance to immunotherapy may develop over time in some patients who initially responded, necessitating research into strategies to overcome this resistance.
There is also a need for a better understanding of how to combine immunotherapy with other cancer treatments (such as chemotherapy, radiation, and surgery) to achieve maximum benefit without unacceptably increasing side effects.
These challenges require continuous research efforts to develop more effective and safer treatments and expand their reach to more beneficiaries.
Final Word
Immunotherapy has truly revolutionized our understanding and ability to fight cancer.
By harnessing the power of the body’s own immune system, this therapeutic approach has offered hope to millions, achieving long-lasting and unprecedented responses in many types of cancers that were previously considered intractable.
Despite the challenges and potential side effects, continuous progress in research and development promises a bright future.
With ongoing research efforts and collaboration between leading global institutions, such as Liva Hospital in Turkey, which invests in the latest immunotherapy technologies, we are getting closer to achieving the ultimate goal: transforming cancer from a fatal disease into a curable condition.
Immunotherapy is not just a new treatment; it is the dawn of a new era in the fight against this complex disease, an era where hope is renewed and patient suffering is diminished.
Frequently Asked Questions
Is immunotherapy the same as chemotherapy?
No, immunotherapy is completely different from chemotherapy. Chemotherapy uses strong drugs to kill rapidly growing cells, including cancer cells and some healthy cells.
What types of cancer can be treated with immunotherapy?
Initially, immunotherapy was effective in treating certain types such as melanoma and lung cancer, but its scope has expanded to now include kidney cancer, bladder cancer, liver cancer, head and neck cancer, colorectal cancer, etc.
Does immunotherapy work for all patients?
Unfortunately, not all patients respond to immunotherapy. The percentage of patients who achieve a lasting response varies depending on the type of cancer, but it usually ranges between 20% and 50% in certain types of cancers.
What are the main side effects of immunotherapy?
The most prominent side effects are immune-related adverse events (irAEs), which occur when the immune system attacks healthy tissues. Common side effects include fatigue, rash, diarrhea, and endocrine gland inflammation (such as thyroiditis).
How long does immunotherapy treatment last?
The duration of immunotherapy varies greatly. It can last for several months or even years in some cases, or until the cancer stops responding, or severe side effects occur. The treating physician determines the appropriate treatment plan for each individual case.
Can immunotherapy be combined with other cancer treatments?
Yes, immunotherapy is often combined with other treatments such as chemotherapy, radiation therapy, or targeted therapy to increase effectiveness and achieve the best results. This combined approach has become a common treatment strategy in many types of cancers.