The removal of the pancreas, or pancreatectomy surgery, is an intervention that involves removing part or all of the pancreas.
The pancreas is considered a vital organ in the body, playing a dual role in secreting digestive enzymes and hormones that regulate blood sugar levels.
However, in some pathological cases, pancreatectomy becomes a medical necessity to save the patient’s life.
It is resorted to only in serious medical cases after accurate diagnosis and is performed in advanced institutions such as Liva Hospital in Turkey, which adopts international protocols and modern surgical techniques.
Main Reasons for Pancreas Removal
The idea of removing an important organ like the pancreas may seem shocking to many, but in some complex medical cases, this step becomes an unavoidable necessity to preserve the patient’s life or improve their quality of life.
We will review in detail the medical reasons that drive doctors to decide on pancreatectomy, based on the latest studies and reliable medical sources.
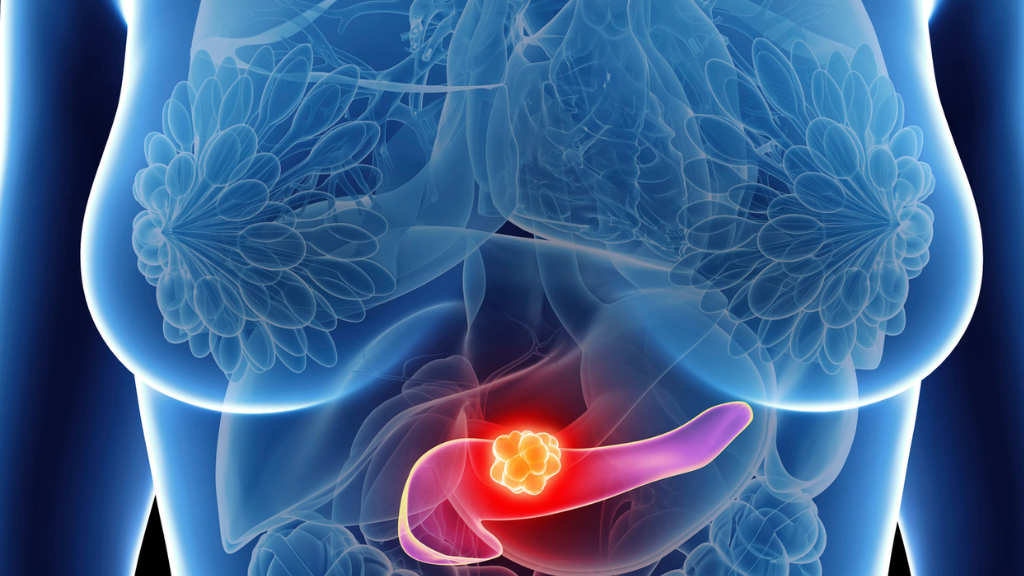
Pancreatic Cancer
Primarily, pancreatic cancer is one of the main reasons for the necessity of pancreas removal.
Ductal adenocarcinoma is common, and in advanced stages, surgery is the only possible curative treatment.
The procedure can be partial (Whipple or pancreatic head resection) or total (pancreatectomy) depending on the tumor’s location and extent of spread.
Chronic Pancreatitis
Sometimes, chronic pancreatitis causes unending pain. Chronic inflammation occurs due to disorders like alcohol abuse or genetic causes, leading to severe pain and complications.
If medication or endoscopic treatments fail to relieve symptoms, pancreatectomy may sometimes be resorted to as a last resort.
A suitable option in some cases is partial pancreatectomy with autologous islet cell transplantation to prevent complete diabetes.
Benign and Precancerous Lesions
Simply put, not all tumors are malignant.
Tumors such as neuroendocrine tumors, cystadenomas/cystadenocarcinomas, and intraductal papillary mucinous neoplasms (IPMN) may require pancreas removal to prevent their transformation or the appearance of symptoms.
When IPMN spreads widely through the ducts, complete surgery is recommended, especially for main duct IPMN.
Multifocal or Hereditary Conditions
Genetics plays a role here.
Conditions such as MEN syndrome, multifocal neuroendocrine tumors, or severe hereditary and multifocal tumors spreading in the pancreas, here, total removal is necessary.
Genetics is unavoidable, but it can be controlled through early surgical intervention.
Complications of Prior Surgery or Pancreatic Leak
Realistically, some failed surgeries require further intervention.
Cases of bleeding or leakage from the pancreatic anastomosis after Whipple surgery may necessitate the removal of the entire pancreas as a salvage procedure.
Severe Trauma or Necrotizing Pancreatitis
Sometimes, severe direct injury occurs, such as blunt trauma to the pancreas. Rare cases require partial or total removal, especially in the presence of severe necrotizing pancreatitis.
Surgical Techniques and Types of Resection
- Total Pancreatectomy: Complete removal of the pancreas, used in advanced cases of cancer or diffuse chronic pancreatitis.
- Whipple Procedure (Pancreaticoduodenectomy): Removes part of the pancreas (the head), and is used for tumors in the head.
- Distal Pancreatectomy: Used for tumors located only in the body or tail of the pancreas.
Life After Removal: Managing Pancreatic Function Loss
Frankly, living afterward requires continuous care. The loss of hormonal and exocrine functions can lead to severe diabetes (Type 1) and a deficiency in digestive enzymes.
About a third of patients may control diabetes after islet cell transplantation. Treatment includes digestive enzymes, diabetes management (insulin), and intensive nutritional follow-up.
Complications of pancreatectomy include:
- Immediate Complications: Bleeding, infection, or pancreatic enzyme leakage (pancreatic fistula).
- Long-Term Complications:
- Diabetes: All patients after total pancreatectomy require insulin.
- Malabsorption: Due to a lack of digestive enzymes, requiring the intake of replacement enzymes.

Pancreatectomy at Liva Hospital in Turkey
Pancreatectomy is a life-saving procedure in cases of malignant tumors or intractable diseases, but it requires an expert surgical team and advanced techniques, as found at Liva Hospital.
With advances in minimally invasive surgeries, the results of these operations have become safer, giving patients a chance for a relatively normal life after surgery.
Liva Hospital provides excellent care using techniques:
- Precise surgery (robotic or laparoscopic) to reduce complications.
- A multidisciplinary team follows up after surgery to adjust blood sugar levels and digestive enzymes.
- Adoption of modern protocols, including autologous islet cell transplantation after pancreatectomy to salvage insulin function in patients with chronic inflammation.
Conclusion
Pancreatectomy is a crucial surgical option in certain cases of chronic cancer, bleeding, or multiple tumors.
The procedure saves the patient’s life, but it comes with lifelong responsibilities, including diabetes and enzyme deficiency.
However, with advanced medical techniques and comprehensive care in centers like Liva Hospital, the quality of life for patients can be maintained after surgery.
Frequently Asked Questions (FAQ)
Does pancreas removal mean the patient will die?
No, it is possible to live for many years without a pancreas using appropriate insulin and digestive enzymes.
When is autologous islet cell transplantation recommended?
It is used after total pancreatectomy in cases of chronic inflammation when sufficient healthy cells are available for transplantation.
What is the difference between partial and total pancreatectomy?
Partial leaves part of the pancreas and reduces complications, while total removes it completely and is used for widespread or severe cases.
Can diabetes be prevented after pancreatectomy?
Not with total pancreatectomy. However, islet transplantation or an artificial pancreas system may improve diabetes control.
What are the complications of pancreatectomy?
They include pancreatic leak, diabetes, enzyme deficiency, nutritional disorders, and the possibility of surgical complications such as infection or bleeding.
Is Liva Hospital a reliable option?
Yes, as Liva adopts international protocols, modern techniques, and a follow-up team for post-surgical cases, it is a good option for those who need this type of operation.