Chronic shoulder pain and limited movement are common health issues that significantly affect many patients’ lives.
The shoulder joint, with its complex structure allowing the widest range of motion among all body joints, becomes susceptible to damage due to years of use, injuries, or degenerative diseases.
When non-surgical treatments fail to provide sufficient relief and restore function, shoulder arthroplasty (shoulder joint replacement) emerges as an effective solution to reconstruct the joint and radically alleviate pain.
This precise surgical procedure is a lifeline for many, as it not only restores their ability to move their arm freely but also gives them a new opportunity to enjoy a more independent and active life.
Below, we’ll delve into everything you need to know about shoulder joint replacement surgery at Liva Hospital, from the reasons that necessitate it to the details of the surgery and recovery, based on the latest reliable medical information.
The Shoulder Joint: Why Does It Get Damaged?
The shoulder joint is a ball-and-socket joint consisting of the head of the humerus (the ball part) which rests within a small socket in the scapula (shoulder blade) known as the glenoid cavity.
This structure gives the shoulder immense flexibility, but also makes it prone to injury and wear.
The joint surfaces are covered with smooth cartilage that allows for frictionless movement.
Joint damage occurs when this cartilage wears away, leading to bones rubbing against each other, causing severe pain, friction, and weakness in movement.
The main causes that lead to shoulder joint damage and necessitate its replacement include:
- Degenerative Arthritis (Osteoarthritis), which is the most common cause where cartilage wears away over time.
- Rheumatoid Arthritis and other types of inflammatory arthritis.
- Avascular Necrosis, where part of the humeral bone dies due to lack of blood supply.
- Severe and complex fractures of the humerus or scapula that cannot be repaired by other methods.
- Lastly, Rotator Cuff Tear Arthropathy, which is joint degeneration due to a chronic and large tear in the rotator cuff tendons.
In shoulder joint replacement surgery, the damaged parts of the joint are replaced with artificial components.
Should You Get a Shoulder Joint Replacement?
Not everyone suffering from shoulder pain is a candidate for joint replacement surgery.
The decision to undergo this surgery depends on a comprehensive and accurate evaluation by an orthopedic surgeon.
You are considered a suitable candidate if you suffer from severe shoulder pain that does not respond to non-surgical treatments, such as anti-inflammatory medications, physical therapy, or cortisone injections.
These pains must significantly impede your ability to perform daily tasks and use your arm normally.
There is no specific age for shoulder replacement surgery, as each case is evaluated individually based on the severity of pain, the degree of disability, and the patient’s general health.
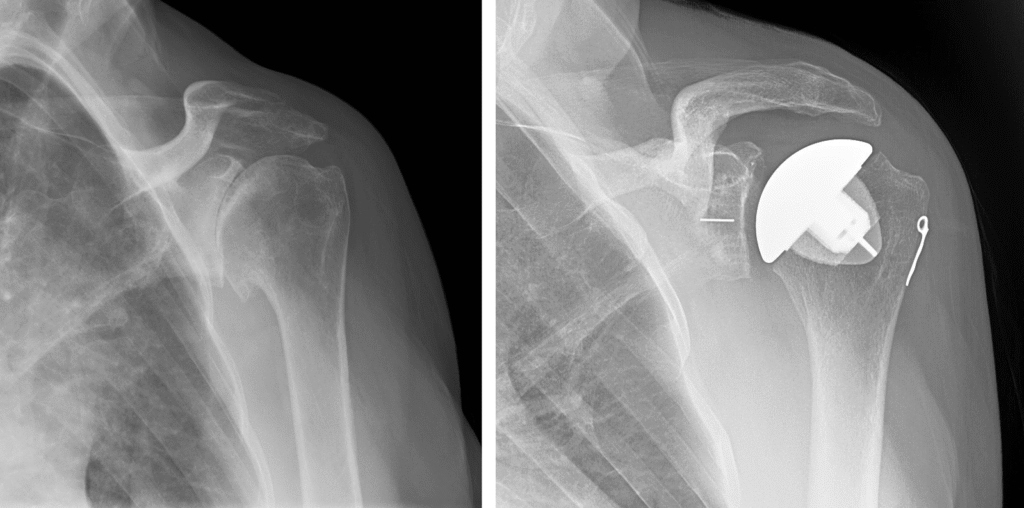
The surgeon will conduct thorough examinations including X-rays, MRI, and CT scans, in addition to a comprehensive evaluation of your medical history.
Muscle strength and shoulder range of motion will also be assessed to determine the most suitable type of surgery for you.
Surgeons at Liva Hospital in Turkey follow strict evaluation protocols to ensure that the operation is the best and safest option for the patient.
Steps for Surgical Preparation
Thorough preparation before shoulder joint replacement surgery is a crucial step towards achieving a successful operation and smooth recovery.
This phase usually begins with a comprehensive health assessment performed by the anesthesiologist and orthopedic surgeon to ensure you are in the best possible health.
These tests may include routine blood tests, electrocardiogram (ECG), and chest X-rays.
It is essential to inform your doctor about all medications, dietary supplements, and herbs you are taking, especially any medications that affect blood clotting, as you may need to stop taking them for a certain period before surgery.
Your doctor may recommend starting a prehabilitation program before surgery to strengthen your shoulder and arm muscles and improve range of motion, which helps accelerate recovery after the operation.
It is also important to plan for the post-surgical phase and arrange for assistance at home during the first few weeks, as your movement will be limited.
It is advisable to stop smoking well in advance of the surgery to improve blood flow and reduce the risk of complications.
Adherence to these guidelines reduces risks and prepares your body and mind for surgery.
Types of Shoulder Joint Replacement Surgery
There isn’t a single “one-size-fits-all” shoulder joint replacement surgery; rather, there are several types that vary depending on the condition of the joint and the extent of damage to the surrounding tendons, especially the rotator cuff.
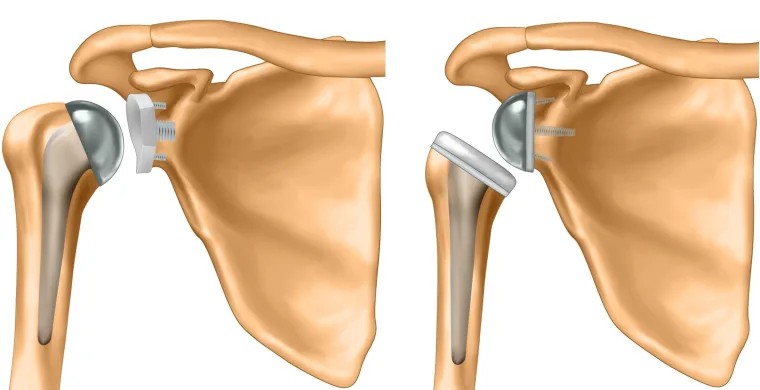
- Anatomic Total Shoulder Arthroplasty (TSA): This is used when the cartilage is worn but the rotator cuff tendons are intact and functional.
In this procedure, the head of the humerus is replaced with a metal head, and the glenoid cavity of the scapula with a smooth plastic component.
This type allows for the restoration of natural shoulder movement thanks to the healthy rotator cuff. - Hemiarthroplasty: In this procedure, only the humeral head is replaced with a metal head, while the natural glenoid cavity remains as is.
This option is usually used in cases of severe humeral head fractures or avascular necrosis when the glenoid cavity is healthy. - Reverse Total Shoulder Arthroplasty (rTSA): This type is an innovative and different option.
In this procedure, the position of the ball and socket is reversed: the metal ball is fixed to the scapula, while the plastic socket is fixed to the humerus.
This type is mainly used for patients suffering from severe shoulder joint degeneration with a large tear in the rotator cuff tendons (Rotator Cuff Tear Arthropathy), where these tendons cannot be used to support the new joint.
This type of surgery relies on the deltoid muscle to provide strength and movement instead of the rotator cuff.
Surgeons, like the experts at Liva Hospital, choose the most appropriate type based on a precise evaluation of the patient’s condition and the type of damage to the joint and surrounding tendons.
Recovery and Rehabilitation Phase
The recovery and rehabilitation phase after shoulder joint replacement surgery is of utmost importance for the success of the operation and the full restoration of arm function.
After surgery, you will feel some pain, which will be effectively controlled using medication. Your arm will be immobilized in a special sling for several weeks for protection and to limit movement.
The physical therapy program begins early, sometimes on the very next day after surgery.
Initially, the physical therapist will teach you gentle passive range of motion exercises (where the therapist moves your arm) to prevent stiffness.
Gradually, you will progress to active range of motion exercises (where you move your arm yourself) and muscle strengthening exercises.
Physical therapy aims to restore full range of motion, strengthen the muscles around the shoulder, and improve balance and coordination.
The rehabilitation program continues for several months, and may last up to a full year to achieve the best results. Adherence to the prescribed exercises, patience, and perseverance are the keys to success in this phase, as your effort will be rewarded with the restoration of your ability to use your arm freely and without pain.
Potential Risks and Complications
Although shoulder joint replacement surgery is safe and successful in most cases, like any major surgical procedure, it carries some potential risks and complications that the patient should be aware of.
Common risks include post-surgical bleeding and infection at the surgical site, which can be treated with antibiotics or, in rare cases, with additional surgery.
Anesthesia-related complications may also occur. Other risks include deep vein thrombosis (DVT) in the arm, which can be prevented by early mobilization and the use of prophylactic medications.
Sometimes, issues related to the artificial joint itself may occur, such as loosening or wear over time, or dislocation, which may necessitate revision surgery in the future.
Less common complications may include damage to nerves or blood vessels in the shoulder area, shoulder stiffness if the physical therapy program is not followed, or chronic pain.
It is very important to discuss all these risks with your surgeon before deciding to undergo the operation, as they will explain how to minimize these risks, thanks to advanced surgical techniques and medical expertise available in specialized centers.
Long-Term: What to Expect?
Shoulder joint replacement surgery provides excellent long-term results for most patients, leading to significant improvement in pain relief, restoration of range of motion, and function.
Studies indicate that most artificial shoulder joints perform well and last for 10 to 15 years or more.
The lifespan of the joint depends on several factors, including the patient’s age, physical activity level, the quality of the joint materials, and the patient’s adherence to post-surgical instructions.
To maintain the new joint for as long as possible, it is advisable to avoid activities that place excessive stress on the shoulder, such as heavy weightlifting or sports that require forceful throwing.
Instead, low-impact activities such as walking, stationary cycling, and swimming are preferred. Regular follow-up with the surgeon is essential to monitor the condition of the joint and detect any signs of early wear or loosening.
Many patients return to their daily activities and favorite hobbies, enjoying a more active and independent life.
Conclusion
Shoulder joint replacement is a critically important surgical procedure that offers a radical solution for millions of people suffering from chronic shoulder pain and loss of function. It is not just a replacement of a damaged joint, but a restoration of freedom of movement and the ability to perform daily tasks that are essential for quality of life.
With continuous advancements in surgical techniques, the diversity of artificial joint types, and integrated rehabilitation programs, this procedure has become safer and more successful than ever before.
From correct diagnosis, selection of the appropriate technique and type, through recovery, to the possibility of re-surgery, all of this represents an interconnected chain that ensures the best results.
And by choosing an excellent center like Liva Hospital, you enjoy a reliable experience focused on quality and safety.
Frequently Asked Questions
Will I need to wear a sling after surgery?
Yes, your arm will typically be placed in a special sling for 2 to 6 weeks after surgery, depending on the type of surgery and your surgeon’s instructions, to protect the joint and allow it to heal.
When can I start using my arm normally after surgery?
Early therapeutic movement begins under the supervision of a physical therapist. Light daily activities usually start after several weeks, and a return to full normal use may take 3 to 6 months, or more depending on the case.
Will I feel any pain after shoulder joint replacement surgery?
It’s normal to feel some pain and swelling after surgery, but it will be effectively managed with prescribed medications. Pain gradually decreases with recovery, and the chronic pain you experienced before surgery disappears in most cases.
Can I play sports after shoulder joint replacement?
You can return to many low-impact sports such as walking, stationary cycling, and swimming after full recovery. It is advisable to avoid high-impact sports or those that require forceful throwing or heavy lifting.
What is the expected lifespan of an artificial shoulder joint?
Studies show that most artificial shoulder joints last for more than 10 to 15 years. The lifespan depends on several factors, including the patient’s age, activity level, and the quality of the materials used.
Can the artificial joint be rejected by the body?
Cases of artificial joint rejection are very rare, as highly biocompatible materials are used. However, complications such as infection or joint loosening over time may occur, which may require medical intervention.



