Have you or a loved one suffered from severe back pain, weakness in movement control, or sensation due to a spinal cord tumor?
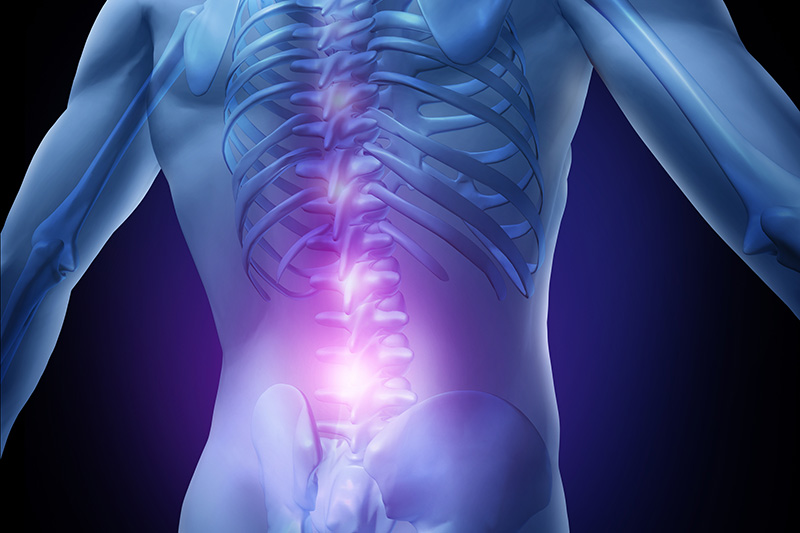
The spinal cord is one of the central nervous system’s fundamental pillars. It acts as the highway transmitting sensory and motor signals between the brain and the rest of the body.
When tumors form within or around the spinal cord, they pose a serious threat to its vital functions.
This can lead to severe pain, limb weakness, numbness, and even paralysis, in addition to loss of body function control.
Spinal cord tumors present a unique surgical challenge due to the sensitivity of this area and its proximity to vital nervous tissues.
In advanced cases, where symptoms are severe or the tumor is growing rapidly, surgical intervention to remove the tumor becomes a crucial option.
It aims to relieve pressure and improve neurological functions.
These operations are performed in reputable centers, including Liva Hospital in Turkey, using the latest neuromonitoring techniques.
Understanding Spinal Cord Tumors
The spinal cord is a vital part of the central nervous system. It’s responsible for transmitting sensory information from the body to the brain and motor commands from the brain to the muscles.
Spinal cord tumors are classified based on their location relative to the dura mater (the membrane surrounding the spinal cord) and their origin:
- Intradural-Extramedullary Tumors: These tumors grow inside the dura mater but outside the spinal cord itself. Meningiomas and Schwannomas are the most common in this category. They are often benign and slow-growing.
- Intramedullary Tumors: These tumors originate within the spinal cord itself. Gliomas, such as Astrocytomas and Ependymomas, are the most common. They can be benign or malignant.
- Extradural Tumors: These tumors grow outside the dura mater. They often arise from the bone surrounding the spine or are metastases from cancers in other parts of the body (such as the lung, breast, or prostate).
Advanced Surgical Techniques for Spinal Cord Tumor Resection
Spinal cord tumor surgery has undergone significant development thanks to technological advancements.
This has allowed neurosurgeons to access complex tumors more safely and accurately. It also reduces risks to the spinal cord and sensitive nerves.
- Laminectomy: This is the most common method for accessing the spinal cord. It involves removing part of the vertebral arch (lamina) from one or more vertebrae above the tumor. This procedure allows the surgeon to directly see the spinal cord and surrounding tumors.
- Discectomy and Fusion: In some cases, especially when the tumor is near the vertebral disc or if there is spinal instability after tumor removal, the disc may be removed, and the affected vertebrae may be stabilized using metal instrumentation (such as screws and rods) to ensure spinal stability after surgery.
- Microscopic Surgery: The use of a high-magnification surgical microscope is indispensable in spinal cord surgery.
The microscope provides a clear and detailed view of tiny blood vessels and nerve fibers. This enables the surgeon to remove the tumor with extreme precision while preserving healthy tissue. - Intraoperative Neuromonitoring (IOM): This technique is crucial for safety during surgery. It is used to continuously monitor the functions of the spinal cord and motor and sensory nerves in real-time.
If any change in nerve signals is observed, the surgeon is alerted to adjust their approach and avoid any potential nerve damage. - Image-Guided Neuronavigation Techniques: Similar to a global positioning system (GPS) for surgery. MRI or CT scans of the brain are used to guide the surgeon with extreme precision to the tumor’s location. This enhances accuracy and reduces collateral damage.
- Minimally Invasive Spine Surgery (MISS) Techniques: In some selected cases, minimally invasive techniques can be used.
These involve smaller incisions and specialized instruments to reduce damage to surrounding muscles and tissues. These techniques can lead to less pain after surgery and a faster recovery period. However, they may not be suitable for all advanced spinal cord tumors. - Laser or Ultrasonic-Assisted Resection: Some advanced tools, such as the laser scalpel or the Ultrasonic Aspirator (CUSA), are used to fragment and aspirate the tumor. This facilitates its removal while reducing pressure on surrounding tissues.
In specialized medical centers like Liva Hospital in Turkey, the use of these advanced is essential to ensure the best surgical outcomes and minimal risks.
Preparing for Spinal Cord Tumor Resection
Comprehensive and meticulous preparation for spinal cord tumor resection is crucial to ensure patient safety and achieve the best possible outcomes.
This stage involves several vital steps that require close coordination among the patient, their family, and the medical team.
- Comprehensive Medical Evaluation: The healthcare team, including the neurosurgeon and anesthesiologist, will perform a series of detailed medical examinations.
These include complete blood tests, an electrocardiogram (ECG), and chest X-rays. This assesses the patient’s general health and ensures their suitability for surgery and anesthesia. - Advanced Diagnostic Imaging: Advanced imaging tests are essential to precisely locate the tumor and its relationship to the spinal cord and surrounding nerves. These tests usually include:
- Spinal MRI with contrast: This is the most important tool for evaluating spinal cord tumors, as it clearly shows the tumor and its borders.
- CT scan: May be performed to evaluate the bones surrounding the tumor.
- Electromyography/Nerve Conduction Studies (EMG/NCS): To assess nerve function before surgery.
- Discontinuing Certain Medications: The patient will be asked to stop taking certain medications that may increase the risk of bleeding during or after surgery.
These include blood thinners (aspirin, warfarin, antiplatelet drugs) or some herbal supplements. This must be done under the doctor’s supervision and within the specified time frame. - Smoking and Alcohol: Smokers are strongly advised to quit smoking several weeks or months before surgery.
Smoking negatively affects wound healing and increases the risk of surgical complications. Alcohol avoidance is also recommended before surgery. - Physical Preparation and Physical Therapy: In some cases, physical therapy may be recommended before surgery to strengthen muscles and improve overall physical fitness. This helps in faster and more effective recovery after the operation.
- Post-Surgery Planning: The medical team discusses post-surgery expectations with the patient and their family.
This includes the potential length of hospital stay, the need for rehabilitation, and any necessary adjustments to the home environment to ensure the patient’s safety and comfort during the recovery period. - Fasting: The patient must refrain from food and drink for a certain number of hours before surgery, according to the anesthesiologist’s instructions, to ensure anesthesia safety.
- Discussion and Education: Fully understanding the surgical procedure, expected risks and benefits, and what to expect during the recovery period is an integral part of preparation.
The patient should ask all questions and concerns to the surgeon and healthcare team to ensure an informed decision and comfort.
What Happens During Spinal Cord Tumor Resection?
Spinal cord tumor resection is a highly precise surgical procedure. It requires exceptional expertise and extensive use of advanced technology to preserve vital neurological functions.
The operation is performed in a specially equipped operating room under general anesthesia.
- Anesthesia and Positioning: After general anesthesia, the patient is carefully positioned on the operating table. This allows the surgeon optimal access to the tumor area in the spine.
The patient’s position is precisely secured to prevent any movement during the operation. - Surgical Incision: The surgeon makes an incision in the skin on the back directly over the tumor area.
The incision size varies based on the tumor’s size, location, and the technique used (open or minimally invasive). - Accessing the Spinal Cord (Laminectomy): The surrounding muscles and tissues are carefully retracted to expose the vertebrae.
The surgeon then removes a portion of the bone (lamina) from the vertebrae covering the tumor.
This is known as laminectomy.
This step provides direct access to the spinal cord and the dura mater (the membrane surrounding the spinal cord). - Dura Mater Opening: The dura mater is carefully opened to expose the spinal cord and intradural tumors. In the case of extradural tumors, opening the dura mater may not be necessary.
- Tumor Localization and Resection: A high-magnification surgical microscope is used. It provides an extremely clear view of the tumor and its relationship to vital nervous tissues.
Neuronavigation and Intraoperative Neuromonitoring (IOM) techniques are continuously used. These guide the surgeon and alert them to any risk to the nerves.
The surgeon carefully resects the tumor. They try to remove as much as possible safely. This preserves the integrity of the spinal cord and nerves. Specialized tools such as the Ultrasonic Aspirator (CUSA) or fine electrocautery may be used. - Bleeding Control: Any bleeding is carefully controlled throughout the operation.
- Incision Closure: After tumor resection and ensuring the area’s stability, the dura mater is carefully closed. In some cases, if bone removal is extensive or there is instability, spinal fusion may be performed.
This uses metal screws and rods to ensure spinal stability. The muscle and tissue layers are then closed, followed by the skin using sutures or surgical staples. - Waking from Anesthesia: The patient is transferred to the recovery room. They are closely monitored until they regain full consciousness and their vital signs stabilize.
Recovery After Spinal Cord Tumor Resection
Recovering from spinal cord tumor resection is a complex and long-term process. It requires patience, specialized care, and a strong commitment to a rehabilitation program.
The recovery path varies significantly among patients based on several factors, including the tumor’s size and location, the extent of neurological damage before surgery, and the patient’s general health.
- Early Stage (In Hospital – Days to Weeks):
- Intensive Care Unit (ICU) and Monitoring: Immediately after surgery, many patients are transferred to the ICU or a neurosurgical post-operative care unit.
This is for close monitoring of neurological functions, blood pressure, respiration, and pain levels.
- Pain Management: Appropriate medications are given to effectively control pain. This ensures patient comfort and aids in early mobilization.
- Continuous Neurological Monitoring: Frequent neurological examinations are performed. This assesses consciousness, strength, sensation, bladder and bowel functions, and any changes in neurological symptoms.
- Early Mobilization and Physical Therapy: The medical team encourages the patient to begin early mobilization, such as sitting and short walks.
This is done with the help of physical therapists, as soon as their condition allows. This helps prevent complications like blood clots and improves circulation.
- Wound Care: Clear instructions are given on how to care for the wound to reduce the risk of infection. Surgical sutures or staples are usually removed after about 7-14 days.
- Intensive Care Unit (ICU) and Monitoring: Immediately after surgery, many patients are transferred to the ICU or a neurosurgical post-operative care unit.
- Intermediate Stage (At Home or Rehabilitation Center – Weeks to Months):
- Intensive Rehabilitation Program: Rehabilitation is the cornerstone of this stage. The patient may need:
- Physical Therapy: To restore muscle strength, improve balance and walking, and enhance mobility.
- Occupational Therapy: To regain skills necessary for daily activities, such as dressing, eating, and bathing.
- Speech Therapy: If the patient’s ability to speak or swallow is affected.
- Symptom Management: The patient may experience fatigue, headaches, or mood changes. These symptoms are managed with appropriate medications and lifestyle advice.
- Regular Medical Follow-up: Regular follow-up visits are conducted with the neurosurgeon and oncologist.
This monitors recovery. It also assesses the need for additional treatments (such as radiation or chemotherapy). And it monitors for any signs of tumor recurrence.
- Gradual Return to Activities: The patient is allowed to gradually return to normal daily activities. However, heavy lifting, excessive bending, or strenuous activities should be avoided until the doctor’s approval.
- Intensive Rehabilitation Program: Rehabilitation is the cornerstone of this stage. The patient may need:
- Late Stage (Months to Years):
- Long-Term Recovery: Recovery and improvement in neurological functions can continue for several months or even years after surgery. Some patients may still experience some mild side effects or disabilities. These may improve with time and continued rehabilitation.
- Long-Term Monitoring: Regular follow-up with the medical team, including periodic spinal imaging, is essential for early detection of any tumor recurrence or development of new complications.
- Psychological Support: Some patients may need psychological support or counseling to adapt to changes after surgery and the challenges of long-term recovery.
At Liva Hospital in Turkey, a comprehensive medical team provides comprehensive and personalized rehabilitation programs for each patient.
This is in close collaboration with physical, occupational, and speech therapists. This ensures effective recovery and improves the patient’s quality of life as much as possible.
Complications of Spinal Cord Tumor Resection
Despite significant advancements in spinal cord surgery, spinal cord tumor resection for advanced cases is a major and precise surgical procedure that carries some potential risks and complications.
The surgeon discusses these risks in detail with the patient and their family before surgery to ensure comprehensive understanding.
- General Anesthesia and Surgery Risks: These risks are associated with any surgical procedure requiring general anesthesia, such as:
- Blood clots: Especially in the legs (deep vein thrombosis), which can travel to the lungs (pulmonary embolism) and be life-threatening.
- Pneumonia or other respiratory problems.
- Allergic reactions: To anesthesia medications or materials used.
- Cardiac problems: Such as irregular heartbeats or heart attack, especially in patients with pre-existing heart conditions.
- Bleeding: Bleeding can occur inside or around the spinal cord during or after surgery. It may require additional surgery or blood transfusion.
- Infection: Infection can occur at the surgical site (skin incision or bone) or inside the spinal canal (meningitis or osteomyelitis). Infection may require strong antibiotics or additional surgery.
- Spinal Cord or Nerve Damage: This is the most serious complication. Although very rare, thanks to advanced intraoperative neuromonitoring techniques. Damage to healthy nervous tissue surrounding the tumor can lead to permanent neurological dysfunction, such as:
- Partial or complete paralysis.
- Worsening of pre-existing weakness or numbness.
- Problems with bladder and bowel functions.
- Loss of sensation.
- Cerebrospinal Fluid (CSF) Leak: In some cases, the fluid surrounding the spinal cord may leak from the surgical site, which can cause headaches or increase the risk of infection. This may require additional surgical repair.
- Pseudomeningocele Formation: Cerebrospinal fluid may collect under the skin at the surgical site, requiring drainage or surgical repair.
- Spinal Instability: In some cases, tumor removal or a large part of the bone may lead to spinal instability, requiring additional stabilization surgery using screws and rods.
- Chronic Pain: Although surgery aims to relieve pain, some patients may continue to experience chronic pain after surgery, either due to pre-existing nerve damage or unknown reasons.
- Tumor Recurrence: Especially in malignant tumors or if the tumor is not completely resected, the tumor can reappear in the same location or in other areas of the nervous system.
The surgical team works to take all possible precautions to minimize these risks. This includes meticulous pre-operative planning, using advanced intraoperative neuromonitoring techniques, and diligent post-operative care.

Outcomes After Spinal Cord Tumor Resection
The outcomes and prognosis after spinal cord tumor resection are affected by several key factors, making them different from patient to patient.
These factors play a crucial role in determining the extent of recovery and long-term quality of life.
- Tumor Type (Benign or Malignant): Benign tumors that can be completely resected have an excellent prognosis in most cases. The patient can achieve complete recovery and return to their normal life.
Malignant tumors have a more complex prognosis. Surgery is often part of a comprehensive treatment plan (with radiation and chemotherapy). It aims to prolong life and improve its quality. It is not a cure in itself in most cases. - Extent of Surgical Resection: The more of the tumor the surgeon can safely remove, the better the prognosis. Complete tumor resection, especially for benign tumors, significantly increases the chances of complete cure and prevents recurrence.
- Tumor Size and Location: Small tumors located in easily accessible areas usually have better outcomes.
Large tumors or those that widely invade the spinal cord or are located in highly sensitive areas may make complete resection difficult and increase the risk of neurological deficit. - Neurological Status Before Surgery: Patients with mild neurological deficits before surgery often have a better prognosis for recovery than those with severe or long-term paralysis. The goal of surgery is to improve symptoms or prevent their deterioration.
- Age and General Health: Younger and generally healthier patients tend to recover better and faster.
- Commitment to Rehabilitation: Adherence to a physical, occupational, and speech therapy program (if necessary) after surgery is crucial for regaining strength, function, and improving long-term outcomes.
- Symptom Improvement: Significant improvement in symptoms related to spinal cord compression (such as pain, weakness, numbness) is observed after surgery in many cases. Some symptoms may take a long time to improve and may not fully heal.
- Quality of Life: Despite physical and psychological challenges, surgery often contributes to an overall improvement in the patient’s quality of life. This is through pain relief, restoration of mobility, and reduced dependence on others.
- Long-Term Follow-up: Regular follow-up with the neurosurgeon and oncologist, including periodic spinal imaging, is essential for early detection of any tumor recurrence or development of new complications.
These prognoses are an area of continuous improvement thanks to ongoing research and advancements in diagnostic and treatment techniques. This gives increasing hope to patients facing these challenges.
Conclusion
Thanks to advancements in diagnostic and surgical techniques, such as intraoperative neuromonitoring, surgical microscopy, and navigation techniques, neurosurgeons can now operate with extreme precision to protect the spinal cord and vital nerves during tumor resection.
Despite the complexity of the procedure, success and improvement rates are good in more than a third of cases.
Meanwhile, outcomes require organized rehabilitation practice and a focus on long-term follow-up. Liva Hospital in Turkey is one of the centers that combines modern techniques and expertise through a multidisciplinary medical team that ensures the best patient care.
The primary goal of this surgery goes beyond merely removing the tumor.
It includes relieving pressure, improving symptoms, restoring neurological functions as much as possible, and in many cases, increasing the chances of recovery and improving the patient’s quality of life.
Frequently Asked Questions
Will my neurological functions fully return to normal after surgery?
This depends on the extent of damage caused by the tumor before surgery, the type of tumor, and the location of the resection. In some cases, significant improvement or even full restoration of functions can occur.
How long will I stay in the hospital after the operation?
The length of hospital stay varies greatly based on the size of the surgery, its complexity, and how quickly the patient recovers.
Will I need intensive physical therapy after surgery?
Yes, in most cases, physical therapy and rehabilitation are a vital part of the recovery process. This therapy helps restore strength, flexibility, balance, and mobility.
What are the risks of paralysis after spinal cord tumor surgery?
Complete paralysis is a very rare complication in modern times, thanks to advanced surgical techniques and intraoperative neuromonitoring. However, there remains a risk of worsening existing weakness or developing new weakness or numbness.
Can the tumor recur after resection?
This depends on the type of tumor. In the case of benign tumors that have been completely resected, the risk of recurrence is very low. For malignant tumors, even after maximal resection, there is always a possibility of tumor recurrence.
Will I feel pain after surgery? How will it be controlled?
Yes, it is normal to feel pain at the surgical site after spinal cord tumor resection. The medical team will provide strong pain medications in the hospital to control it effectively.