Have you or a loved one experienced chronic pain or weakness in your spine and wondered about surgical treatment options?
Let’s be frank: back pain is a global health issue affecting millions, ranging from mild discomfort to debilitating pain that hinders daily activities.
The spine, this complex structure that supports the body and protects the spinal cord, is often the source of this pain.
While most back problems can be managed with non-surgical treatments like physical therapy and medication, certain conditions necessitate surgical intervention to restore stability and relieve nerve compression.
Among these interventions, spinal fusion stands out as a major surgical procedure aimed at joining two or more vertebrae into a single, solid bone mass.
This procedure is a crucial option for patients suffering from spinal instability, structural deformities, or chronic pain resulting from degenerative disc disease.
Understanding the Spine
To understand the need for spinal fusion, it’s essential first to explore the structure and function of the spine.
The spine consists of a series of vertebrae (bones) separated by flexible intervertebral discs, which act as cushions and shock absorbers and allow movement.
Within the spinal canal, formed by the vertebrae, runs the spinal cord, from which nerves branch out to supply the rest of the body.
When this vital structure is damaged, whether due to injury, natural wear and tear with aging, or certain diseases, it can lead to severe pain, weakness, or even disability.
Spinal fusion is a primary surgical option in specific cases where non-surgical treatments have failed to provide adequate relief or when there is an urgent need to restore spinal stability. The main indications for this procedure include:
- Spinal Instability: This occurs when vertebrae are unstable and move excessively, causing pain and potentially compressing the spinal cord or nerves. This can result from vertebral fractures, spondylolisthesis (slippage of one vertebra over another), or severe disc degeneration.
- Spinal Deformities: Such as severe scoliosis (an abnormal sideways curvature of the spine) or kyphosis (an excessive forward curvature). In these cases, fusion aims to correct the curvature, maintain that correction, and reduce pain.
- Severe Degenerative Disc Disease: When an intervertebral disc significantly deteriorates and loses its shock-absorbing capacity, causing chronic back pain that may radiate to the limbs (radiculopathy). Fusion works by removing the source of pain by joining the affected vertebrae.
- Spinal Stenosis: Narrowing of the spinal canal through which the spinal cord and nerves pass, causing compression and pain. In some cases, fusion may be necessary after decompression surgery (such as laminectomy) to maintain spinal stability and prevent its deterioration.
- Spinal Tumors or Infections: Removal of tumors or treatment of infections may require the removal of parts of the vertebrae, necessitating fusion to restore the spine’s structural stability.
Spinal Fusion Techniques
Spinal fusion techniques have significantly evolved over the years, making them more precise and safer.
All methods aim to achieve the primary goal: fusing two or more vertebrae into a single, solid bone mass. However, surgical approaches differ in how they access the spine and the materials used to achieve this fusion.
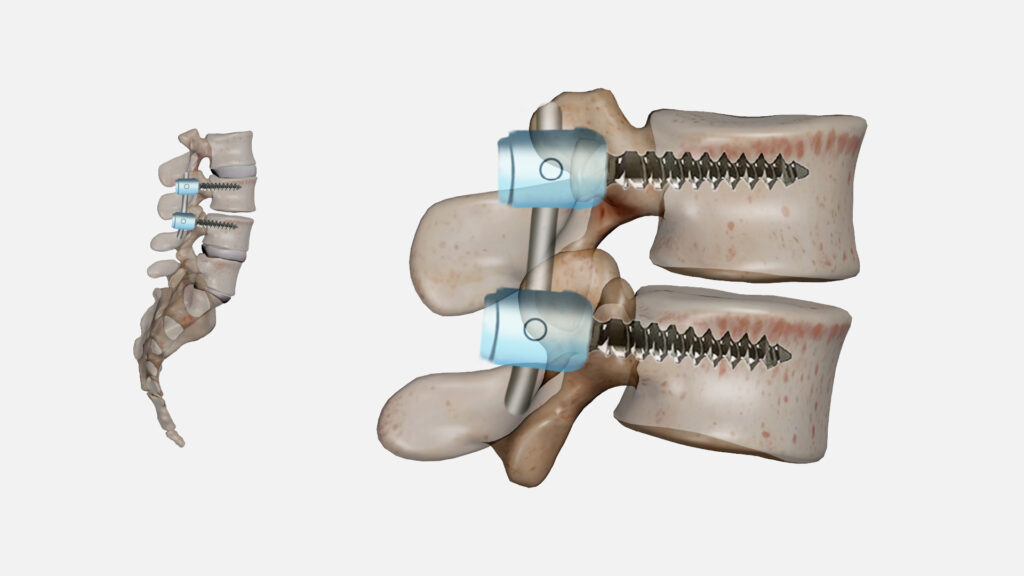
- Posterior Approach: These are the most common approaches. A surgical incision is made in the middle of the back, and the spine is accessed from the rear. In these methods, metal screws and rods (usually made of titanium) are often used to temporarily stabilize the vertebrae while new bone grows between them.
- Posterior Lumbar Fusion (PLF): Commonly used to fuse vertebrae in the lower back.
- Posterior Lumbar Interbody Fusion (PLIF): Involves removing the damaged disc from the back and placing a bone graft or cage between the vertebrae to encourage fusion.
- Transforaminal Lumbar Interbody Fusion (TLIF): Similar to PLIF but involves accessing the disc from one side to avoid excessive manipulation of nerves, which may reduce the risk of neurological complications.
- Anterior Approach: In these methods, a surgical incision is made from the front (from the abdomen for lumbar spine, or from the neck for cervical spine).
- Anterior Cervical Discectomy and Fusion (ACDF): This is one of the most common neck surgeries, where the damaged disc is removed from the front and replaced with a bone graft or cage to fuse the vertebrae.
- Anterior Lumbar Interbody Fusion (ALIF): Used in the lower back, it allows for complete disc removal and the placement of a large bone graft, providing a larger surface for fusion and reducing damage to the posterior muscles.
- Lateral Approach: These methods are used to access the spine from the side, reducing the need to retract large muscles or nerves.
- Oblique Lumbar Interbody Fusion (OLIF): Performed from the anterolateral side, providing good access to the disc while minimizing manipulation of blood vessels and nerves.
- Lateral Lumbar Interbody Fusion (LLIF or XLIF): Accessed from the patient’s right or left side.
- Minimally Invasive Spine Surgery (MISS) Techniques: These techniques aim to achieve the same goals as open surgery but with much smaller incisions, less damage to surrounding tissues, and a faster recovery period. Specialized instruments and small cameras (endoscopes) are used to perform the operation with high precision.
Preparing for Spinal Fusion Surgery
Thorough and advanced preparation for spinal fusion surgery is crucial for its success and for achieving a smooth and effective recovery.
This preparation usually begins weeks or even months before the surgery date and includes a comprehensive set of medical examinations and preventive instructions.
- Comprehensive Medical Evaluation: A specialized medical team, including the anesthesiologist and spine surgeon, will conduct a series of comprehensive medical examinations to ensure the patient is medically fit for surgery.
This includes routine blood tests, an electrocardiogram (ECG) to assess heart health, and chest X-rays. Any pre-existing chronic health conditions such as heart disease, diabetes, or high blood pressure, are evaluated and effectively managed before surgery to minimize risks. - Medication Cessation: The patient may be asked to stop taking certain medications that can increase the risk of bleeding during or after surgery.
This includes blood thinners such as aspirin and warfarin, as well as some herbal supplements and vitamins, for a specific period before surgery as determined by the doctor. - Smoking Cessation: Quitting smoking is crucial for smokers before undergoing spinal fusion.
Smoking significantly reduces the chances of successful bone healing and vertebral fusion (non-union is one of the biggest risks) and also increases the risk of post-surgical complications such as infection and respiratory problems.
It is recommended to quit smoking several weeks or even months before surgery. - Physical Preparation: Physical therapy may be recommended before surgery to strengthen core muscles and improve the patient’s overall physical fitness. This physical preparation helps in faster and more effective recovery after surgery.
- Post-Surgery Logistics Arrangements: The patient and their family are advised to arrange for support and assistance at home after surgery, as the patient will need help with daily activities during the initial recovery period.
It is preferable to prepare a safe environment for recovery, such as removing rugs that may cause tripping and placing essential items within reach to avoid excessive bending. - Fasting: The patient must refrain from food and drink for a certain number of hours before surgery, according to the anesthesiologist’s instructions, to ensure anesthesia safety.
- Discussion and Education: Fully understanding the surgical procedure, expected risks and benefits, and what to expect during the recovery period is an integral part of preparation.
The patient should ask all questions and concerns to the surgeon and healthcare team before surgery to ensure an informed decision and comfort.
What Happens During Spinal Fusion Surgery?
Spinal fusion surgery is usually performed in an operating room under full general anesthesia.
The exact course of the operation varies depending on the surgical technique used and the number of vertebrae to be fused, but the basic steps are shared across most approaches:
- Anesthesia and Positioning: After general anesthesia, the patient is positioned appropriately for surgery.
For example, if a posterior approach is used, the patient will be placed on their stomach, while for an anterior approach, they will be on their back. The surgical area is then thoroughly cleaned and sterilized to reduce the risk of infection. - Surgical Incision and Access: The surgeon makes an incision through the skin and muscles to access the spine. In traditional open techniques, the incision is larger to allow for a wider view.
In minimally invasive techniques, incisions are much smaller, and an endoscope or advanced surgical microscope is used to guide the surgeon and clearly visualize the target area. - Removal of Damaged or Compressing Tissues: If there is a damaged intervertebral disc, a bone spur (osteophyte), or a part of the vertebra compressing the spinal cord or nerves, it is carefully removed using precise surgical instruments. This aims to relieve pressure on the nerve structures causing pain.
- Preparing the Fusion Site: The surfaces of the vertebrae to be fused are scraped.
This scraping aims to remove any cartilaginous remnants and stimulate bleeding from the bone, providing an environment rich in factors that encourage new bone growth and fusion of the vertebrae. - Bone Graft Placement: A bone graft (which can be from the patient’s own body, from a donor, or synthetic materials) is placed in the space between or around the vertebrae.
This graft acts as a bridge through which new bone grows to fuse the vertebrae. - Instrumentation: Metal screws and rods (usually made of titanium), or plates and screws in the neck region, are used to hold the vertebrae in their correct position and prevent them from moving during the bone healing process.
These instruments act as temporary internal supports and provide immediate spinal stability. - Incision Closure: Once the instrumentation is complete and the integrity of the neural structures is ensured, the layers of tissue and muscle, then the skin, are closed using sutures or surgical staples.
- Waking from Anesthesia: The patient is transferred to the recovery room where they are closely monitored by the anesthesia and nursing team until they fully regain consciousness and their vital signs stabilize.
Recovery After Spinal Fusion Surgery
Recovering from spinal fusion surgery is a multi-stage journey that requires patience, adherence to doctors’ instructions, and active participation in a rehabilitation program.
The recovery timeline varies significantly from person to person based on factors such as the extent of surgery, age, and the patient’s overall health.
- Early Stage (First few days to weeks after surgery):
- Hospital Stay: The patient typically stays in the hospital for 2 to 5 days, depending on the type of surgery, its complexity, and the speed of initial recovery.
- Pain Management: Appropriate medications are given to control pain after surgery to ensure patient comfort and aid in early mobilization.
- Early Mobilization: Doctors encourage early and light movement (such as short walks) with the assistance of the physical therapy team. This helps reduce the risk of complications like blood clots (deep vein thrombosis) and improves circulation.
- Physical Therapy: Physical therapy often begins in the hospital, where the patient learns how to get out of bed, walk safely, and perform basic daily activities in a way that does not jeopardize the spine.
- Brace: Some patients may be required to wear a special back or neck brace to support the spine and provide additional stability during the initial fusion process.
- Intermediate Stage (Few weeks to a few months after surgery):
- Regular Physical Therapy: Regular and consistent physical therapy is vital at this stage. The program focuses on strengthening core and back muscles, improving balance, and gradually and safely restoring range of motion.
- Activity Restriction: The patient must continue to avoid activities that place significant stress on the spine, such as heavy lifting, excessive bending, twisting, and high-impact activities.
- Return to Light Activities: Gradual return to light activities such as longer walks, driving (after doctor’s approval), and returning to desk work if possible.
- Late Stage (Several months to a year or more after surgery):
- Complete Bone Fusion: The complete bone fusion process usually takes between 6 months to a year, and sometimes longer in certain cases. The surgeon monitors the fusion process using periodic X-rays to ensure new bone growth and fusion stability.
- Return to Normal Activities: Once the surgeon confirms sufficient fusion, the patient can gradually return to most normal activities, including exercise and hobbies. However, it may be advised to permanently avoid some high-impact activities or those requiring strong twisting to protect the spine in the long term.
- Ongoing Pain Management: Some mild pain or discomfort may persist for a period after surgery and can be managed with prescribed medications or guided physical therapy.
Specialized doctors at Liva Hospital in Turkey are committed to providing a comprehensive post-operative care plan, including intensive physical therapy sessions and regular follow-up.
Potential Risks and Complications
Although spinal fusion is considered a safe and effective procedure when performed by highly experienced surgeons, like any major surgery, it carries some potential risks and complications.
It is important for patients to be aware of these risks and discuss them fully with their surgeon before deciding to undergo surgery.
- General Anesthesia and Surgery Risks: These include common risks associated with any surgical procedure requiring general anesthesia, such as:
- Blood clots: Especially in the legs (deep vein thrombosis), which can travel to the lungs (pulmonary embolism) and be life-threatening.
- Respiratory problems: Such as pneumonia.
- Allergic reactions: To anesthesia medications or materials used.
- Cardiac problems: Such as heart attack or irregular heartbeats, especially in patients with pre-existing heart conditions.
- Bleeding: Can occur during or after surgery and may require blood transfusion in some cases.
- Infection: Infection can occur at the surgical site (superficial or deep) and may require antibiotics or additional surgery in rare cases to clean the area.
- Nerve or Spinal Cord Damage: Although extremely rare thanks to advanced intraoperative neuromonitoring techniques, this is the most serious potential complication.
Damage to nerves or the spinal cord can lead to weakness, numbness, partial or complete paralysis, or loss of bladder and bowel control. - Failure of Fusion (Pseudarthrosis): Occurs when the vertebrae do not fully fuse to form a solid bone mass.
This can lead to persistent or recurring pain and may require another surgery to fix it. These risks significantly increase in smokers, uncontrolled diabetics, and those with osteoporosis. - Persistent Pain: Although the fusion is successful, some patients may continue to experience chronic pain after surgery, either due to pre-existing nerve damage or unknown reasons.
- Problems with Implanted Hardware: In rare cases, screws or rods may break or move out of place, which can cause pain or fusion failure and require surgery to fix or remove them.
- Adjacent Segment Disease: After fusing a part of the spine, mechanical stress on the adjacent discs and vertebrae to the fused segment may increase.
This increased stress can lead to degeneration of these vertebrae and the development of new problems (such as stenosis or disc herniation) in the future, which may require additional surgery.

Outcomes and Prognosis After Spinal Fusion Surgery
Spinal fusion aims to achieve significant improvement in the patient’s quality of life by effectively reducing pain, restoring spinal stability, and correcting structural deformities.
However, it is important to have realistic expectations about the potential outcomes.
- Pain Improvement: Significant improvement in pain is observed in the majority of patients after spinal fusion, especially pain associated with instability or direct nerve compression.
However, it is important to realize that not all pain may completely disappear, especially if the patient has long-term chronic pain. - Restoration of Function: Most patients can gradually return to their normal activity levels after a full recovery period.
This includes the ability to walk for longer periods, perform daily activities more comfortably, and return to work. However, it may be advised to permanently avoid some high-impact activities or those requiring strong twisting to protect the spine. - Fusion Success Rate: The success rate of bone fusion (i.e., the vertebrae joining together to form a single bone mass) is high, around 85-95% in most recent studies.
However, this rate is affected by factors such as smoking, other health conditions, and patient compliance with post-operative instructions. - Importance of Rehabilitation: Adherence to the prescribed physical therapy and rehabilitation program after surgery is crucial for achieving the best long-term results.
This program helps restore muscle strength, improve flexibility, and enhance balance, enabling the patient to regain full functional movement. - Impact on Quality of Life: Generally, the majority of patients who undergo successful spinal fusion report a significant improvement in their quality of life.
This includes increased ability to participate in social activities, pursue hobbies, reduce reliance on pain medication, and improve overall psychological well-being due to chronic pain relief.
Comprehensive Cost in Turkey
According to medical sources, the cost of fusing a single lumbar vertebra using open techniques in Turkey ranges between $5,000 and $30,000 USD, depending on the level of technology used, the hospital’s standards, and additional services.
MISS or robotic techniques may have a slightly higher initial cost, but they reduce the length of stay and care costs, making them more economically viable compared to the same procedures in the United States or Europe.
It is important to note that each case is unique and may require other costs in addition to the basic surgical costs in the hospital.
Conclusion
Spinal fusion is a complex and effective surgical procedure that provides a lasting solution for a variety of spinal problems causing severe pain and disability.
From instability and spinal deformities to advanced degenerative disc disease, this surgery offers patients a chance to restore function, reduce pain, and significantly improve their quality of life.
While the procedure requires meticulous preparation and a long recovery path,
Liva Hospital is one of the leading centers in Turkey in the field of spinal surgery.
We feature a technological array that includes open surgery, minimally invasive techniques, and endoscopy, in addition to using 3D navigation devices to improve fusion outcomes and ensure patient safety.
Frequently Asked Questions
Will my mobility be affected after spinal fusion surgery?
Yes, some movement will be lost in the fused part of the spine because the vertebrae will be joined to become a single bone mass.
How long does full recovery take?
Full recovery after spinal fusion surgery takes between 6 months to a full year, and sometimes longer.
Can I exercise after spinal fusion surgery?
Generally, yes, but only after complete recovery and with your doctor’s approval.
Can fusion fail after surgery?
Yes, there is a possibility of fusion failure (pseudarthrosis), meaning the vertebrae do not fully fuse to form a solid bone mass. This occurs in a small percentage of cases (about 5-15%).
Can airport metal detectors be triggered by the implanted hardware?
In most cases, the screws and rods used in spinal fusion, which are usually made of titanium, do not trigger airport metal detectors because titanium is not magnetic.
Will the pain after surgery be severe?
Pain after surgery is expected, and the healthcare team will provide strong pain medication to control it during your hospital stay.



