For every child born with heart problems, don’t despair… there’s immense hope in the tremendous progress of modern medicine.
While most children are born with healthy hearts that pump life smoothly, some face complex congenital defects that require precise medical intervention.
Among these defects, Tetralogy of Fallot (TOF) is one of the most common and complex cyanotic congenital heart defects (those causing blueness of the skin and lips).
It’s a condition that hinders the normal flow of blood from the heart to the lungs and then to the rest of the body, forcing parents and medical teams to confront a crucial decision: surgery.
Tetralogy of Fallot surgery is a life-saving surgical procedure that restores vital heart functions, enabling children to live normal, active lives, offering hope for a strong heart that keeps pace with their dreams.
TOF surgeries are routinely performed at Liva Hospital in Turkey by a specialized surgical team that uses the latest techniques to build a healthy future for affected children.

What is Tetralogy of Fallot?
Tetralogy of Fallot is a congenital heart defect that a child is born with, classified as a cyanotic heart defect due to the lack of oxygen in the blood, which causes blueness of the skin.
It’s called “tetralogy” because it consists of four main structural defects that occur together and impede normal blood flow:
- Pulmonary Stenosis (Narrowing of the Pulmonary Valve or Artery): This is the most prominent defect and is responsible for most of the symptoms.
The pulmonary valve (which regulates blood flow from the right ventricle to the pulmonary artery and then to the lungs) or the area beneath it becomes narrow, making it difficult for deoxygenated blood to reach the lungs for oxygenation. - Ventricular Septal Defect (VSD): There is a large hole in the wall (septum) separating the right and left ventricles.
This hole allows oxygen-rich blood from the left ventricle to mix with oxygen-poor blood from the right ventricle, and this mixed blood is then pumped to the body. - Overriding Aorta: The aorta (the largest artery carrying oxygenated blood to the body) does not emerge normally only from the left ventricle, but directly over the ventricular septal defect, allowing it to receive mixed blood from both ventricles.
- Right Ventricular Hypertrophy (Enlargement of the Right Ventricle): Due to the increased pressure the right ventricle faces to pump blood through the narrowed pulmonary valve, its walls become abnormally thick and muscular.
Diagnosing Tetralogy of Fallot
Early diagnosis of Tetralogy of Fallot is crucial for determining the optimal timing for surgical intervention and improving long-term outcomes.
TOF is often detected at an early stage, sometimes even before birth or immediately after birth:
- Prenatal Diagnosis: Tetralogy of Fallot can sometimes be detected during routine prenatal ultrasound examinations (fetal echocardiogram), giving parents and the medical team time to prepare and develop a treatment plan.
- Post-Natal Diagnosis: Common symptoms that raise suspicion include:
- Cyanosis: Bluish discoloration of the lips, nails, and skin, which may be evident when crying or feeding.
- Tet Spells: Sudden and severe episodes of cyanosis, where the child becomes pale, agitated, and may lose consciousness. These spells usually occur during crying, feeding, or exertion.
- Heart Murmur: An abnormal sound heard by the doctor with a stethoscope.
- Difficulty feeding or slow weight gain.
- Shortness of breath and panting.
Several tests are used to confirm the diagnosis:
- Echocardiogram: This is the primary test for diagnosing Tetralogy of Fallot. It provides detailed images of the heart, its valves, and blood flow through it, clearly showing the four defects.
- Electrocardiogram (ECG): Records the electrical activity of the heart and can show right ventricular hypertrophy.
- Chest X-ray: May show a heart with a distinctive size and shape (resembling a “boot”).
- Cardiac Catheterization or Cardiac MRI: These more detailed tests may be used in some cases to assess the complexity of the defects before surgery.
What is the Optimal Timing for the Operation?
This decision is made by a specialized team in congenital heart diseases, considering the child’s general health, the severity of the defects, and the progression of symptoms.
The timing of Tetralogy of Fallot surgery is a critical decision determined by several factors, and surgery is usually preferred at an early age to avoid long-term complications.
- Optimal Age: In most cases, complete corrective surgery for Tetralogy of Fallot is performed when the child is between 3 to 6 months of age, or when the child reaches 5 kilograms in weight. Studies indicate that performing surgery at this age improves long-term outcomes and reduces the risk of complications.
- Severe Tet Spells: If the child suffers from recurrent and severe tet spells that do not respond to medical treatment, surgery may become necessary at a very early age, even if the child is only a few weeks old.
These spells indicate a severe lack of oxygen and pose a risk to the brain. - Child’s Growth and Development: If Tetralogy of Fallot is impeding the child’s growth and development (such as insufficient weight gain), early surgery may be necessary to improve their general health.
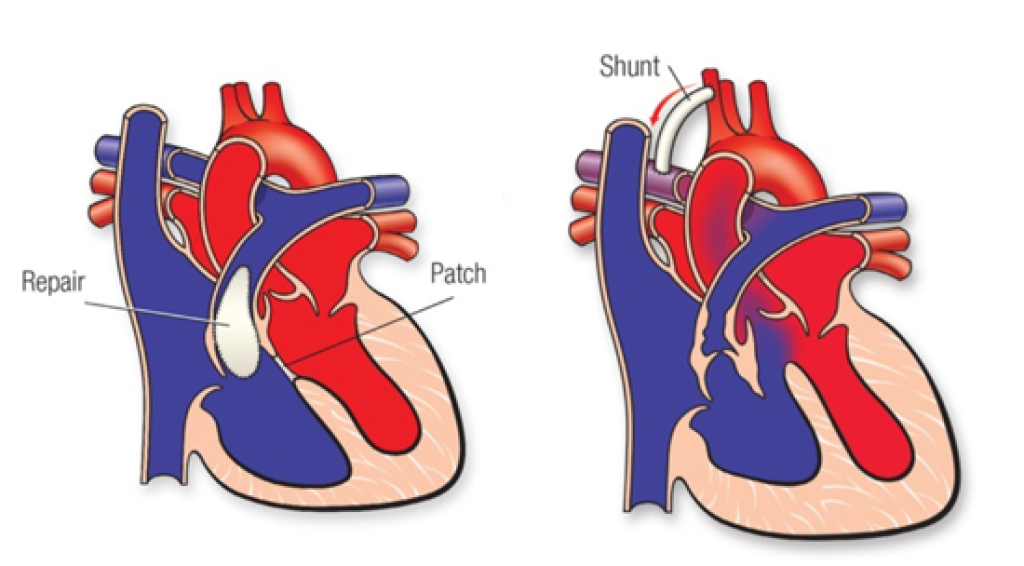
- Specific Heart Anatomy: In some rare cases where the pulmonary arteries are not sufficiently developed, doctors may recommend a preliminary palliative surgery (such as a shunt procedure) to improve blood flow to the lungs, followed by complete corrective surgery at a later stage.
Details of Tetralogy of Fallot Surgery to Correct Congenital Defects
Tetralogy of Fallot surgery is a complex surgical procedure performed under general anesthesia, usually using a Heart-Lung Machine which temporarily takes over the functions of the heart and lungs to allow the surgeon to operate on a still heart.
After repairing the defects, the child is weaned off the heart-lung machine, and the heart begins to function normally.
At Liva Hospital in Turkey, these precise operations are performed by surgeons specializing in pediatric cardiac surgery, using the latest techniques to ensure the best outcomes for young Tetralogy of Fallot patients. The goal is to achieve the maximum possible normal heart function, reduce cyanosis, and improve the child’s long-term quality of life.
After surgery, the child is placed in the Pediatric Intensive Care Unit (PICU) for close monitoring.
Doctors and nurses monitor vital signs, organ functions, and any signs of complications. Medications are given to aid heart function, control pain, and prevent infection.
The post-surgical care team has extensive experience in managing these potential complications to ensure the best chance of recovery.
The operation aims to correct the four main defects:
- Widening the Pulmonary Outflow Tract: The surgeon widens the narrowed pulmonary valve and pulmonary artery.
This may involve removing part of the thickened muscle beneath the valve (right ventricular hypertrophy) or enlarging the pulmonary valve annulus. In some cases, a patch is used to widen the pulmonary artery or valve. - Closing the Ventricular Septal Defect (VSD Repair): The large hole between the ventricles is closed using a patch (usually made of synthetic material or specialized tissue).
This prevents blood mixing between the ventricles and ensures that oxygenated blood is pumped to the body and deoxygenated blood is pumped to the lungs. - Adjusting the Overriding Aorta: After closing the ventricular septal defect, the aorta will exclusively receive oxygenated blood from the left ventricle.
Potential Risks and Complications
Although Tetralogy of Fallot surgery is considered very safe today thanks to medical advancements, it is still a major surgery and carries some potential risks and complications that parents should be aware of:
- Bleeding: May occur during or after surgery.
- Infection: At the wound site or inside the body.
- Heart Rhythm Problems (Arrhythmias): Heart rhythm disturbances may develop after surgery, usually temporary and manageable with medication.
- Residual Leak or Narrowing: In some rare cases, the repair may not be perfect, and a small leak or slight narrowing may remain, which may require additional intervention in the future.
- Problems with Other Organ Functions: Such as the kidneys or lungs, especially in the first few days after surgery.
- Stroke: Rare but possible.
Recovery and Long-Term Care for the Child
The recovery period after Tetralogy of Fallot surgery is a long journey that requires patience and meticulous care, but it leads to significant improvement in the child’s health and quality of life.
- Hospital Stay: The child usually remains in the hospital for one to two weeks after surgery, including a few days in the intensive care unit.
- Home Recovery: After discharge from the hospital, the child needs a home recovery period that lasts several weeks. Strenuous activities and exposure to illness should be avoided. Doctors provide detailed instructions on wound care, medications, and nutrition.
- Gradual Improvement: Over time, a noticeable improvement in the child will be observed; cyanosis will disappear, the child will become more active, and will start gaining weight and growing normally.
- Long-Term Follow-up: Children who have undergone Tetralogy of Fallot surgery should have lifelong follow-up with a cardiologist specializing in congenital heart disease.
Regular examinations (such as echocardiogram, electrocardiogram, and sometimes stress tests or MRI) are performed to monitor heart function, pulmonary valve, and pulmonary artery pathway.
Some patients may experience residual problems such as Pulmonary Regurgitation or Arrhythmias that may require further follow-up or interventions in the future.
However, the vast majority of children who have undergone corrective surgery for Tetralogy of Fallot live normal and active lives and can participate in most sports activities after consulting their doctor.
Conclusion
Tetralogy of Fallot surgery is one of the shining success stories in pediatric cardiac surgery.
This complex condition, which was once fatal, has been effectively treated thanks to amazing medical advancements.
It highlights the vital role of early diagnosis, specialized surgical expertise, and comprehensive pre- and post-operative care.
By correcting the four defects in the heart, the child’s normal blood flow is restored, cyanosis disappears, and they can live with a heart that beats with strength and hope.
Every child cured of Tetralogy of Fallot is a living testament to the potential of modern medicine to save lives and renew hope.
In this field, Liva Hospital in Turkey enjoys a strong reputation and advanced use of the best expertise and techniques, to ensure optimal results for each individual case.
Frequently Asked Questions
Can a child live with a completely healthy heart after Tetralogy of Fallot surgery?
After complete corrective surgery, the heart functions close to normal. However, patients who have undergone Tetralogy of Fallot surgery are considered to have “adult congenital heart disease” and require lifelong follow-up with a cardiologist.
What are Tet Spells, and how can they be managed?
Tet Spells are sudden episodes of severe oxygen deficiency causing bluish discoloration of the skin and pallor. They usually occur during crying or exertion.
Will there be a large scar after the operation?
Yes, Tetralogy of Fallot surgery is usually performed through an incision in the middle of the chest to open the breastbone. There will be a scar, but over time and as the child grows, it will become less noticeable.
Can the child participate in sports after the operation?
In most cases, children who have undergone complete corrective Tetralogy of Fallot surgery can participate in most sports activities after full recovery and consultation with their cardiologist.
What are the most common long-term complications after Tetralogy of Fallot surgery?
The most common long-term complications include pulmonary regurgitation, heart rhythm disturbances (arrhythmias), and pulmonary artery dilation. These complications can often be managed with medication or may require additional interventions in the future.
What is the average life expectancy for people who have undergone Tetralogy of Fallot surgery?
Thanks to advancements in surgery and post-operative care, the vast majority of individuals who have undergone Tetralogy of Fallot surgery live into adulthood and old age, enjoying a good quality of life, although they require ongoing medical follow-up.