The urinary system is a vital system in the human body, responsible for filtering blood from toxins and waste, producing urine, and maintaining fluid and electrolyte balance.
Despite its extreme importance, this system is not immune to tumors, whether benign or malignant.
Urological tumors represent a wide range of diseases that can affect any part of this system, including the kidneys, ureters, bladder, and urethra, in addition to the prostate gland in men.
Dealing with these tumors requires a deep understanding of their different types, accurate diagnostic methods, and various advanced treatment options.
Approaches vary depending on the type and stage of the tumor, but advanced equipment and multidisciplinary teams—like those at Liva Hospital—play a crucial role in improving outcomes and restoring hope to patients.
Common Types of Urological Tumors
Urological tumors vary in nature and location, necessitating a deep understanding of each type to determine the optimal treatment approach. The most prominent of these tumors include:
- Kidney Cancer: Renal Cell Carcinoma (RCC) is the most common type. It’s often discovered incidentally during imaging tests for other reasons in its early stages. Risk factors include obesity, smoking, and high blood pressure.
Symptoms range from no symptoms in early stages to blood in the urine, flank pain, or an abdominal mass in advanced stages. - Bladder Cancer: This is the most common cancer in the urinary system. It usually originates from the cells lining the bladder (transitional cells).
Smoking is the most significant risk factor, in addition to exposure to certain chemicals. The most common symptom is painless blood in the urine, which may be visible (gross hematuria) or microscopic. - Prostate Cancer: This is one of the most common types of cancer among men, originating in the prostate gland.
Its development is influenced by factors such as age, family history, and ethnicity. In its early stages, there may be no symptoms, but as the disease progresses, it may cause urination problems, erectile dysfunction, or bone pain if it spreads. - Ureteral and Urethral Cancers: These types are less common than the ones mentioned above.
Ureteral cancer originates in the tubes that carry urine from the kidneys to the bladder, while urethral cancer originates in the tube that carries urine out of the body.
Symptoms are usually similar to bladder cancer, such as blood in the urine or pain during urination.
Symptoms and Warning Signs: When to Consult a Doctor?
Awareness of the symptoms and warning signs of urological tumors is a crucial first step towards early diagnosis, which plays a pivotal role in treatment success.
Although many of these symptoms may be caused by benign conditions, their appearance warrants immediate medical consultation. The most common symptoms include:
- Blood in the urine (Hematuria): The presence of blood in the urine, whether visible to the naked eye (urine appears red, pink, or tea-colored) or microscopic (detected only by laboratory examination), is the most important warning sign for urological tumors, especially bladder, kidney, and ureteral cancer.
- Changes in urination habits: Such as increased frequency of urination, urgent need to urinate, pain or burning during urination (Dysuria), or a weak urine stream, especially in men (may indicate prostate problems).
- Pain: The patient may experience persistent pain in the flank, lower back, or pelvis, which may indicate a kidney, bladder, or prostate tumor in advanced stages.
- Palpable mass: In some cases, especially with large kidney tumors, a mass may be felt in the abdominal or flank area.
- General symptoms: Such as unexplained fatigue, unexplained weight loss, or persistent fever, which may indicate an advanced stage of cancer.
The Accurate Diagnosis
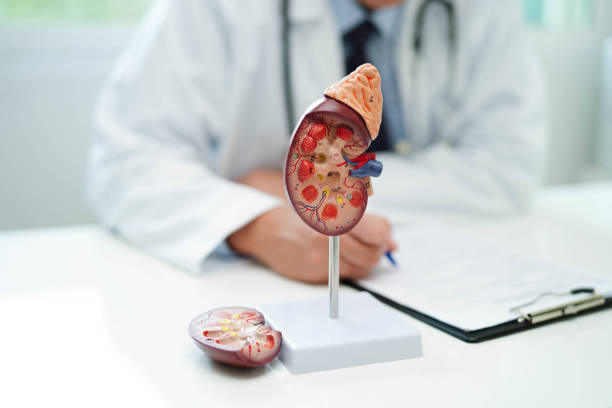
Accurate diagnosis of urological tumors is the cornerstone of developing an effective treatment plan.
The diagnostic process usually begins with a comprehensive review of the patient’s medical history and a physical examination.
This is followed by a set of specialized tests that help identify the presence, type, size, and stage of the tumor’s spread:
- Urinalysis and Urine Culture: To detect the presence of blood, abnormal cells, or infection.
- Imaging Tests: These tests are essential for determining the tumor’s location and size. They include:
- Ultrasound: Fast, non-invasive, and useful for initial detection of kidney, bladder, and prostate tumors.
- CT Scan (Computed Tomography): Provides detailed images of internal organs and is used to assess tumor size and its spread to lymph nodes or adjacent organs.
- MRI (Magnetic Resonance Imaging): Provides clearer images of soft tissues and is often used to evaluate prostate and bladder tumors and to determine if the tumor has spread outside the organ.
- Intravenous Pyelogram (IVP) or CT Urogram: To evaluate the ureters and bladder.
- Cystoscopy: A procedure where a thin tube with a camera is inserted through the urethra into the bladder to directly examine the bladder lining and take biopsies of any suspicious areas.
- Biopsy: This is the crucial step to confirm the diagnosis. A small tissue sample is taken from the suspicious area and examined under a microscope to determine if it contains cancer cells and their type.
Biopsies can be taken during endoscopy, using an imaging-guided needle (for kidney and prostate tumors), or during surgery. - PSA Test (Prostate-Specific Antigen): Used as an early screening tool for prostate cancer and to monitor treatment effectiveness.
Treatment Options for Urological Tumors
Treatment options for urological tumors have evolved significantly, offering a comprehensive and personalized approach that matches the type, stage, and general health of the patient. The most prominent of these options include:
- Surgery: Surgery is the cornerstone in the treatment of many urological tumors and aims to completely remove the tumor. Different types include:
- Nephrectomy: To remove the cancerous kidney, which can be partial (removing part of the kidney) or radical (removing the entire kidney). It is often performed using laparoscopic or robotic surgery to reduce recovery time.
- Cystectomy: To remove the bladder affected by advanced bladder cancer. It can be partial or radical (removing the entire bladder and sometimes adjacent organs).
- Prostatectomy: To remove the prostate gland affected by cancer, often performed laparoscopically or robotically.
- Transurethral Resection of Bladder Tumor (TURBT): For superficial bladder cancer, where the tumor is removed through the urethra.
- Ureteral and Urethral Tumor Resection: The surgical procedure is determined based on the tumor’s location and size.
- Radiation Therapy: Uses high-energy rays to kill cancer cells or reduce tumor size. It can be used as a primary treatment (especially for prostate cancer), after surgery (adjuvant therapy), or to relieve symptoms (palliative therapy).
- Chemotherapy: Uses drugs to kill cancer cells throughout the body. It is typically used in cases of advanced or metastatic cancer, or after surgery to reduce the risk of tumor recurrence. It can be given intravenously or orally.
- Immunotherapy: Boosts the body’s immune system to fight cancer cells. It is used for some types of advanced kidney and bladder cancer.
- Targeted Therapy: These drugs target specific molecules involved in the growth and spread of cancer cells, minimizing damage to healthy cells. It is used for some cases of advanced kidney cancer.
- Intravesical Therapy: For non-muscle invasive bladder cancer, drugs (such as BCG or chemotherapy) are injected directly into the bladder to kill cancer cells and prevent tumor recurrence.
These treatments are often given in an integrated manner (e.g., surgery followed by chemotherapy or radiation therapy) to increase the chances of a cure.
In leading medical institutions like Liva Hospital in Turkey, a multidisciplinary team of urologists, oncologists, radiologists, and pathologists collaborate to develop an individualized treatment plan for each patient.
Supportive Care and Follow-up
Managing urological tumors is not limited to effective treatment; it extends to include Supportive Care and Follow-up, which are integral parts of the comprehensive recovery journey.
Supportive care aims to improve the patient’s quality of life during and after treatment, by managing medication side effects, dealing with pain, and providing psychological and social support.
This may include involving nutritionists to adjust the diet, physical therapists to restore strength and motor function, and psychological counselors to help the patient adapt to the emotional challenges of the disease.
Regular follow-up, on the other hand, is essential for early detection of any signs of tumor recurrence (relapse) or development of long-term complications.
Follow-up usually includes regular imaging tests (such as CT scans), blood tests including the PSA test for prostate cancer, urine tests, and bladder endoscopy in cases of bladder cancer.
The frequency and intensity of these tests vary based on the type of tumor, its stage, and the type of treatment the patient received.
This regular follow-up is the cornerstone of maintaining the patient’s long-term health and gives the medical staff the opportunity to intervene quickly if any abnormal indicators appear, which enhances the chances of achieving sustained positive results.
Prevention and Awareness
Prevention and awareness of urological tumors are among the most important strategies for reducing incidence rates and improving early detection opportunities.
Although some risk factors cannot be controlled (such as family history or genetics), there are many factors that can be modified to reduce risks:
- Quitting smoking: Smoking is the most important major risk factor for bladder and kidney cancer. Quitting it significantly reduces the risk.
- Maintaining a healthy weight: Obesity increases the risk of kidney cancer.
- Controlling blood pressure: High blood pressure is a risk factor for kidney cancer.
- Avoiding exposure to chemicals: Some professions involving exposure to certain chemicals (such as dyes) increase the risk of bladder cancer.
- Following a healthy diet: Rich in fruits and vegetables, and low in fat.
- Drinking enough water: May help reduce the risk of some urological tumors.

Final Word
Urological tumors represent a complex health challenge that requires a holistic and precise approach to diagnosis and treatment.
From common kidney and bladder cancers to prostate cancer specifically affecting men, these tumors vary in nature.
However, tremendous advancements in diagnostic techniques and advanced treatment options, including precise surgery (such as robotic surgery) and innovative drug therapies like immunotherapy give patients renewed hope.
The role of leading medical centers like Liva Hospital in Turkey, which combine specialized expertise with the latest equipment, is invaluable in providing excellent care for this group of patients.
Frequently Asked Questions
Are all urological tumors cancerous?
No, not all tumors are cancerous (malignant). There are also benign tumors that can affect the urinary system, but any tumor must be carefully evaluated to determine its nature.
Is regular screening necessary for early detection of urological tumors?
Yes, regular screening is important, especially if you have risk factors. For example, PSA screening for prostate cancer is recommended for men in certain age groups, and regular urine tests may be recommended for smokers or those exposed to certain chemicals.
Can urological tumors be treated without surgery?
It depends on the type of tumor, its stage, and its location. Some tumors may respond to radiation therapy, chemotherapy, immunotherapy, or targeted therapy, without the need for major surgery, especially in advanced stages or if surgery is not possible.
What are the common side effects of urological cancer treatments?
Side effects vary depending on the type of treatment. Surgery may cause pain, infection, or bleeding. Chemotherapy and radiation therapy may cause fatigue, nausea, hair loss, or irritation of the skin or mucous membranes.
Will I need to change my lifestyle after treatment?
It is often recommended to adopt a healthy lifestyle that includes a balanced diet, regular exercise, and avoiding smoking and alcohol. Some cases may require permanent lifestyle changes, especially if a large part of the urinary system has been removed.
What are the chances of recovery from urological tumors?
The chances of recovery depend largely on the type of cancer, the stage of its detection, the patient’s general health, and their response to treatment. Early diagnosis and appropriate treatment significantly increase cure rates and survival.