When a patient faces a diagnosis of complex diseases affecting the pancreas, duodenum, bile duct, or nearby parts of the stomach, the treatment prospects can seem grim.
However, there is an exceptional and complex surgical procedure that offers a significant glimmer of hope for those with these conditions: Whipple Procedure, also known as Pancreaticoduodenectomy.
This operation is considered one of the most intricate surgical procedures, requiring extreme precision, superior surgical skill, and a multidisciplinary medical team.
Despite its challenges, the Whipple procedure has proven effective in improving survival rates and quality of life for many patients.
In fact, this operation is the only option for treating tumors in the head of the pancreas and the proximal part of the bile duct, and it is performed in highly competent centers such as Liva Hospital in Turkey, which provides precise techniques and expert surgeons.
Reasons for Whipple Surgery
The Whipple procedure is the primary surgical option for many conditions affecting the head of the pancreas, the duodenum, the common bile duct, or part of the stomach.
The most common reason for this operation is pancreatic cancer, specifically tumors originating in the head of the pancreas.
Pancreatic cancer is considered an aggressive cancer often discovered in late stages, and the Whipple procedure offers the greatest hope for a complete cure if the tumors are resectable.
The decision to perform a Whipple procedure requires a meticulous and comprehensive evaluation of each case, considering the tumor’s location, size, extent of spread, and the patient’s general health.
In addition to pancreatic cancer, the Whipple procedure is also performed to treat other types of cancers affecting the region, such as duodenal cancer, distal bile duct cancer, and ampullary cancer.
Beyond malignant tumors, the Whipple procedure may be performed to treat certain premalignant lesions that could turn cancerous, or for non-cancerous diseases that cause serious complications, such as:
- Severe chronic pancreatitis that does not respond to other treatments.
- Neuroendocrine tumors in the pancreas.
- Large pancreatic cysts that carry a risk of malignant transformation.
What Happens During Whipple Surgery?
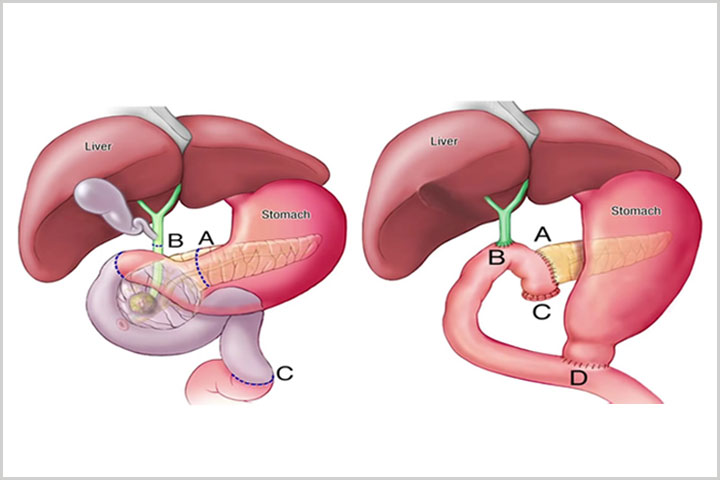
The Whipple procedure is one of the most complex surgical operations because it involves removing and reconnecting multiple parts of the digestive system in a very precise manner. The operation typically involves the following steps:
- Removal of the head of the pancreas: This is the part connected to the duodenum and located near the main bile duct.
- Removal of the duodenum: This is the first part of the small intestine that wraps around the head of the pancreas.
- Removal of part of the common bile duct: This is the duct that carries bile from the liver and gallbladder to the intestines.
- Removal of the gallbladder: Due to its connection to the bile duct, a portion of which is resected.
- Removal of part of the stomach: In some cases, especially if the tumor is close to the stomach outlet (this is known as the classic or standard Whipple resection).
- Reconstruction of the digestive system: After removing the affected parts, the surgeon re-connects the remaining pancreas, bile duct, and stomach (if not removed) to the small intestine (jejunum) in a way that ensures the continuous flow of digestive enzymes and bile into the intestines naturally.
These steps require extreme precision to prevent leakage or complications.
The remaining part of the pancreas is usually connected first to the jejunum (Pancreaticojejunostomy), then the bile duct (Hepaticojejunostomy), and finally the stomach (Gastrojejunostomy).
The anatomical complexity of this procedure necessitates highly experienced surgeons and a comprehensive medical team to ensure the highest levels of precision and safety.
Preparation and Post-Surgical Care
Given the complexity of the Whipple procedure, both the pre-surgical preparation and post-surgical care phases are crucial for the success of the procedure and the patient’s recovery.
The preparation phase begins with a comprehensive and in-depth assessment of the patient’s health, including detailed laboratory tests and advanced imaging studies such as CT scans and MRI to evaluate the tumor, its extent of spread, and its relationship to major blood vessels.
The patient may be asked to stop certain medications, such as blood thinners, before surgery. Good pre-surgical nutrition is also critically important, and the patient may be given nutritional supplements to support their health.
Psychological counseling is also provided to the patient and their family to help them understand the procedure and the challenges they may face.
Post-surgical care is intensive and continues for several days or even weeks in the hospital.
The patient is transferred to the intensive care unit or a critical monitoring room immediately after surgery for close monitoring of their vital signs.
Care includes effective pain management, monitoring of digestive system functions, and blood sugar level monitoring, as pancreatic function may be affected. Gradual fluid intake is started, followed by soft foods, until the digestive system returns to its normal function.
Physical therapy and proper nutrition play a significant role in rapid recovery and regaining strength.
Psychological support for the patient and their family is also an integral part of comprehensive care to ensure the best possible outcomes.
Potential Complications and How to Manage Them
Despite significant advancements in Whipple surgery techniques, it still carries some potential risks and complications due to its complexity and the sensitivity of the organs involved. The most prominent complications include:
- Pancreatic Leak: This is one of the most serious complications, where digestive pancreatic fluids can leak from the site where the pancreas is connected to the intestine, leading to inflammation or infection.
- Hemorrhage: Either during or after surgery.
- Infection: At the wound site or inside the abdomen.
- Delayed Gastric Emptying: Where the stomach takes longer than usual to empty its contents after surgery.
- Bile Duct Problems: Such as stricture or bile leakage.
- Diabetes: Pancreatic function in insulin production may be affected, which could lead to the onset or worsening of diabetes.
Managing these complications requires high expertise and a multidisciplinary team.
The focus is on preventing them through good preparation, surgical precision, and continuous monitoring after the operation.
In international centers such as Liva Hospital in Turkey, operating rooms are equipped with the latest technologies, and highly experienced medical teams are available to handle such complex cases, contributing to reducing the complication rate and improving survival rates.
Recent Advances in Whipple Surgery
The Whipple procedure has seen significant advancements in recent years, leading to improved outcomes and reduced mortality and complication rates.
The most notable of these advancements include:
- Minimally Invasive Surgery: This includes Laparoscopic Whipple and Robotic Whipple. In robotic surgery, the surgeon uses a robotic system that provides magnified 3D vision and superior maneuverability, allowing the operation to be performed through very small incisions.
These techniques reduce post-surgical pain, accelerate recovery, and shorten hospital stays compared to traditional open surgery. - Improved Reconstruction Techniques: Research and trials have led to the development of better techniques for re-connecting the pancreas and other organs, reducing the risk of pancreatic leak, which is one of the most serious complications.
- Multidisciplinary Care: It has become essential for a multidisciplinary team to be involved in the care of a Whipple patient, including specialized surgeons, anesthesiologists, nutritionists, critical care specialists, and oncologists. This approach ensures comprehensive and integrated patient care.
- Enhanced Recovery After Surgery (ERAS): These are modern care protocols aimed at accelerating patient recovery by focusing on early nutrition, early mobilization, and effective pain management.
Conclusion
In conclusion, the Whipple procedure is a complex and challenging surgical intervention that requires exceptional skill and extreme precision.
However, it simultaneously represents a significant glimmer of hope for patients suffering from serious tumors and diseases affecting the pancreas, duodenum, and bile duct.
Despite potential risks and complications, the continuous development in surgical techniques, the increasing experience of specialized medical teams, and the multidisciplinary approach to care have all contributed to significantly improving the outcomes of this operation.
The presence of distinguished medical centers such as Liva Hospital in Turkey, which provides the latest equipment and trained medical staff, gives patients a real chance for recovery and improved quality of life.
Frequently Asked Questions
Is the Whipple procedure the only treatment for pancreatic cancer?
Not always. The Whipple procedure is the primary surgical treatment for tumors originating in the head of the pancreas or resectable tumors. In some cases, chemotherapy or radiation therapy may be used before or after surgery.
How long does full recovery take after a Whipple procedure?
Recovery varies from person to person, but it usually takes several weeks to a few months (from 6 to 12 weeks or more) for complete recovery and restoration of normal energy levels.
Will I need to take pancreatic enzymes after the operation?
In most cases, yes. Because part of the pancreas is removed, the body may not produce enough digestive enzymes, necessitating the intake of pancreatic enzyme supplements to help digest food and absorb nutrients.
Will I develop diabetes after a Whipple procedure?
Not all patients develop diabetes after a Whipple procedure. It depends on the amount of remaining pancreatic tissue and its function. However, some patients may develop diabetes or experience worsening of their pre-existing condition, requiring continuous monitoring of blood sugar levels.
What about the diet after a Whipple procedure?
Initially, there will be a gradual dietary progression. In the long term, a low-fat, high-protein diet is recommended, with small, frequent meals. Personalized dietary guidance may be provided by a nutritionist.
Can the Whipple procedure be performed laparoscopically or robotically?
Yes, laparoscopic and robotic surgery have become available options for performing the Whipple procedure in specialized centers, which reduces the size of surgical incisions and speeds up recovery. However, they still require significant surgical expertise.