The heart is the essence of life, acting as a complex orchestra that coordinates the rhythm of blood throughout the body.
But sometimes, this orchestra may experience a disruption in its rhythm, leading to what is known as cardiac arrhythmias.
These disorders can range from a mere sensation of palpitations to serious, life-threatening conditions where the electrical signals that regulate the heart’s beats become irregular, too fast, or too slow.
In the past, treatment relied heavily on medication, but with significant advancements in cardiology, more precise and effective solutions have emerged.
One of the most prominent of these solutions is cardiac ablation, scientifically known as an Electrophysiology Study (EPS) and Ablation.
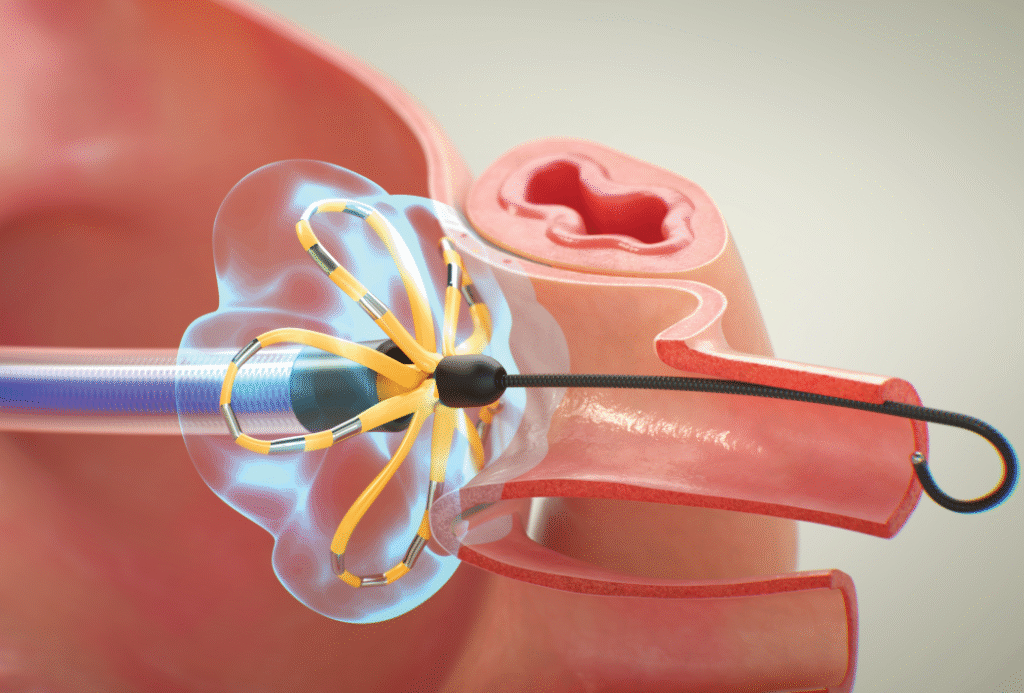
This precise procedure involves guiding a catheter to the heart to identify the source of the malfunction and treat it.
It’s available in advanced centers like Liva Hospital in Turkey, utilizing the latest equipment and under the supervision of a comprehensive cardiac team.

Understanding Arrhythmias
The heart is a pulsating muscle managed by a complex electrical system that generates and transmits electrical signals, regulating its contractions and relaxations.
These signals are known as the “heart’s electrical system.” When this system malfunctions, the heart’s function is affected, and cardiac arrhythmias appear.
Arrhythmias are classified based on their origin and heart rate:
- Supraventricular Tachycardia (SVT): These arrhythmias originate in the atria or the atrioventricular node and include:
- Atrial Fibrillation (AFib): The most common type of arrhythmia, where the atria beat rapidly and irregularly, hindering blood flow and increasing the risk of strokes.
- Atrial Flutter: Rapid and relatively regular atrial beats.
- Atrial Tachycardia.
- Wolff-Parkinson-White Syndrome (WPW).
- Ventricular Tachycardia (VT): These arrhythmias originate in the ventricles and are more serious, as they can cause reduced blood flow to the body and may lead to sudden cardiac arrest.
- Bradycardia: Very slow heartbeats.
Heart Conditions and Indications for Cardiac Ablation
Cardiac ablation, usually preceded by an Electrophysiology Study (EPS), is an effective treatment option for patients suffering from arrhythmias that do not respond to medication.
The main indications for cardiac ablation include:
- Refractory Atrial Fibrillation: When medications fail to control atrial fibrillation, or when medications cause unacceptable side effects.
- Atrial Flutter.
- Various types of Supraventricular Tachycardia.
- Ventricular Tachycardia: Especially for patients who cannot be controlled with medication or who experience recurrent episodes.
- Wolff-Parkinson-White Syndrome (WPW).
- Stroke Prevention: In certain cases of atrial fibrillation where the risk of stroke is high, cardiac ablation may help reduce this risk.
Techniques of Cardiac Ablation
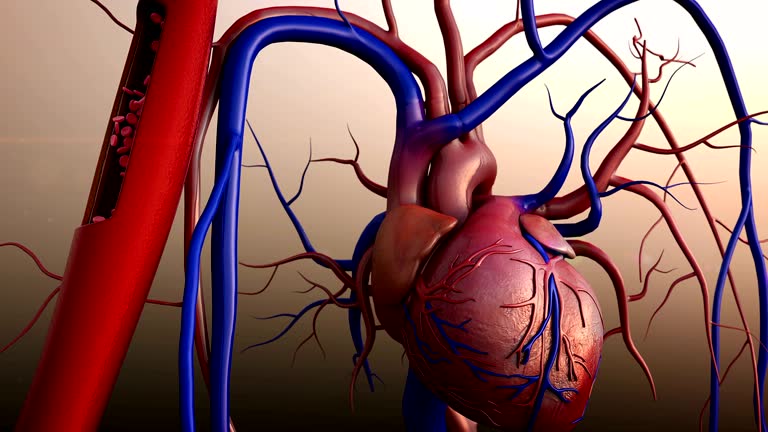
After precisely identifying the source of the arrhythmia through an Electrophysiology Study (EPS), the cardiac ablation procedure begins.
The goal is to destroy the cardiac cells responsible for generating or transmitting abnormal electrical signals, thereby disrupting the abnormal electrical pathway and resetting the heart’s rhythm.
Two main ablation techniques are used:
- Radiofrequency Ablation (RFA):
- This is the most common technique.
- A special ablation catheter is used, whose small tip is heated using radiofrequency energy (a high-frequency electrical energy).
- When the catheter tip touches the targeted cardiac tissue, the heat creates a small scar (ablation). This scar isolates the area responsible for the abnormal electrical signals, preventing them from spreading.
- It’s like burning a small road on a map to prevent vehicles from passing.
- Cryoablation:
- This technique is used in some cases, especially in the treatment of certain types of supraventricular tachycardia and atrial fibrillation (particularly pulmonary vein isolation).
- Instead of heat, a catheter releases a very cold cooling agent (usually nitrous oxide) to freeze and destroy the targeted cells.
- The advantage of cryoablation is that it allows for “testing” the effect of freezing before causing permanent tissue destruction. If the result is undesirable, the freezing can be reversed, and the tissue returns to its normal state.
Recovery After Cardiac Ablation
Since cardiac ablation is a catheter-based procedure, the recovery period is faster and less painful compared to open surgery.
Most patients can return to their normal lives within a few days.
- Early Stage (In-hospital – hours to one day):
- Monitoring: After the procedure, the patient is transferred to a monitoring room, where vital signs, blood pressure, and the access site are closely monitored to prevent any bleeding.
- Rest: The patient is asked to rest in bed with the leg through which the catheter was inserted kept straight for several hours (usually 4-6 hours) to prevent bleeding at the access site.
- Pain and Discomfort: The patient may feel some mild pain or bruising at the access site, or mild chest pain, which can be controlled with over-the-counter pain relievers.
- Nausea and Fatigue: Some patients may experience mild nausea or a feeling of fatigue, but these are usually temporary.
- Hospital Discharge: In most cases, the patient can be discharged from the hospital on the same day or the morning after, once their condition stabilizes.
- Intermediate Stage (At home – days to weeks):
- Access Site Care: The access site should be kept clean and dry to avoid infection. Avoid rubbing the area vigorously. There may be a small bruise or mild swelling that gradually disappears.
- Physical Activity: It is advised to avoid heavy lifting or strenuous physical activities, or swimming pools and taking showers instead of baths for several days to a week. Light walking can be gradually resumed.
- Medications: The doctor will provide clear instructions regarding medications to continue taking (especially blood thinners if the patient has atrial fibrillation) and any new medications.
- Post-Procedure Symptoms: Some patients may experience palpitations or irregular heartbeats in the first few days or weeks after ablation. This is normal and known as the “honeymoon period,” and it may take some time for the treated tissues to stabilize.
- Long-Term Stage (Weeks to months):
- Regular Follow-up: Regular follow-up with an electrophysiologist is essential to assess the success of the procedure, monitor heart rhythm, and perform electrocardiograms or Holter monitoring for long-term surveillance.
- Final Results: It may take several weeks to a few months to fully evaluate the final results of the ablation.
- Lifestyle: Maintaining a heart-healthy lifestyle is advised, including a balanced diet, regular exercise, and stress management.
Potential Risks and Complications
Although cardiac ablation is considered safe and effective, like any medical procedure, it carries some potential risks and complications.
These complications are relatively rare, but it is important for patients to be aware of them and discuss them with their doctor.
- Risks Associated with the Access Site (Groin):
- Bleeding or Severe Bruising: These are the most common, and usually mild. In rare cases, bleeding can be severe and require intervention.
- Hematoma Formation: A collection of blood under the skin.
- Infection: At the access site, which is rare.
- Artery or Vein Damage: Puncture or damage to blood vessels rarely occurs.
- Heart-Related Risks:
- Pericardial Effusion/Tamponade: Fluid accumulation around the heart or pressure on the heart due to fluid. This complication is serious but very rare (less than 1%) and occurs if the heart wall is accidentally punctured by the catheter. It may require fluid drainage or emergency surgery.
- Coronary Artery Damage: Ablation rarely affects the coronary arteries that supply the heart, which could cause a heart attack.
- Heart Valve Damage: The catheter rarely causes damage to the heart valves.
- Damage to the Natural Electrical Conduction System: Ablation may affect the atrioventricular (AV) node or other pathways, causing slow heartbeats and requiring permanent pacemaker implantation, especially if the treated area is close to these vital structures.
- Blood Clots and Stroke: Although rare, a blood clot may form on the catheter tip or in the heart and travel to the brain (causing a stroke) or to other parts of the body. Blood thinners are used during the procedure to reduce this risk.
- General Risks:
- Radiation Exposure: From X-rays used for guidance. Although the dose is relatively low, it is taken into consideration.
- Allergic Reactions: To anesthesia medications or dyes.
- Kidney Problems: In rare cases, the dye used in X-rays may cause temporary kidney damage.
Conclusion
Cardiac ablation (EPS and Ablation) is a remarkable medical achievement, offering a precise and effective solution for arrhythmias that previously caused significant suffering for patients and drastically reduced their quality of life.
This advanced technique has transformed arrhythmia treatment from mere symptom management with medication to the possibility of a complete cure in many cases.
The ability to identify the exact source of irregular electrical signals and destroy them with extreme precision, thanks to 3D mapping systems and advanced ablation techniques, represents a paradigm shift in cardiology.
Although the procedure requires careful preparation and a simple recovery period, the potential benefits of restoring a normal heart rhythm and returning to an active life justify these efforts.
Leading international hospitals, such as Liva Hospital in Turkey, offer the highest levels of expertise and technology in this field, ensuring the best possible outcomes for patients.
Frequently Asked Questions
Is cardiac ablation a definitive cure for all arrhythmias?
Cardiac ablation is highly effective, especially for certain types of supraventricular tachycardia and atrial flutter, achieving very high cure rates. However, its effectiveness can vary depending on the specific type and complexity of the arrhythmia.
Will I be awake during the procedure?
The procedure is usually performed under local anesthesia with light sedation to help you relax and be comfortable. You may be vaguely aware of your surroundings, but won’t feel pain.
How long does cardiac ablation take?
The duration of the procedure varies depending on the type and number of arrhythmias being treated. Generally, it can range from 2 to 4 hours, but complex cases (like atrial fibrillation) may take longer.
When can I return to work or normal activities after the procedure?
Most patients can return to light daily activities within two to three days after the procedure. It is advised to avoid heavy lifting or strenuous physical activities for several days to a week to ensure the access site heals. Your doctor will provide detailed instructions.
Will I need to take blood thinners after the procedure?
This depends on the type of arrhythmia treated and your other risk factors. If you have atrial fibrillation, you will often need to continue taking blood thinners (such as warfarin or newer oral anticoagulants) to prevent blood clots.
Can arrhythmias return after ablation?
Although ablation is very effective, there is a small chance of the arrhythmia recurring over time. This can happen if not all abnormal cells were destroyed in the first session, or if new foci develop. In such cases, a repeat ablation or other treatments might be considered.