Arterial diseases, from narrowing to aneurysms, have long presented a significant challenge for surgeons and physicians.
Indeed, they often require major surgical interventions to save limbs or even lives.
However, the last two decades have witnessed a true revolution in vascular treatment, thanks to the emergence and development of endovascular procedures, also known as the “closed approach.”
These innovative methods, performed via a small catheter through a tiny incision, have changed the game, offering a less invasive alternative to traditional open surgery.
They enable doctors to access damaged arteries from within, repairing or “replacing” them with high effectiveness, significantly reducing pain and recovery time, thereby restoring hope to millions of patients in regaining their quality of life.
What Is Endovascular Techniques?
Endovascular techniques represent a paradigm shift in the treatment of arterial diseases.
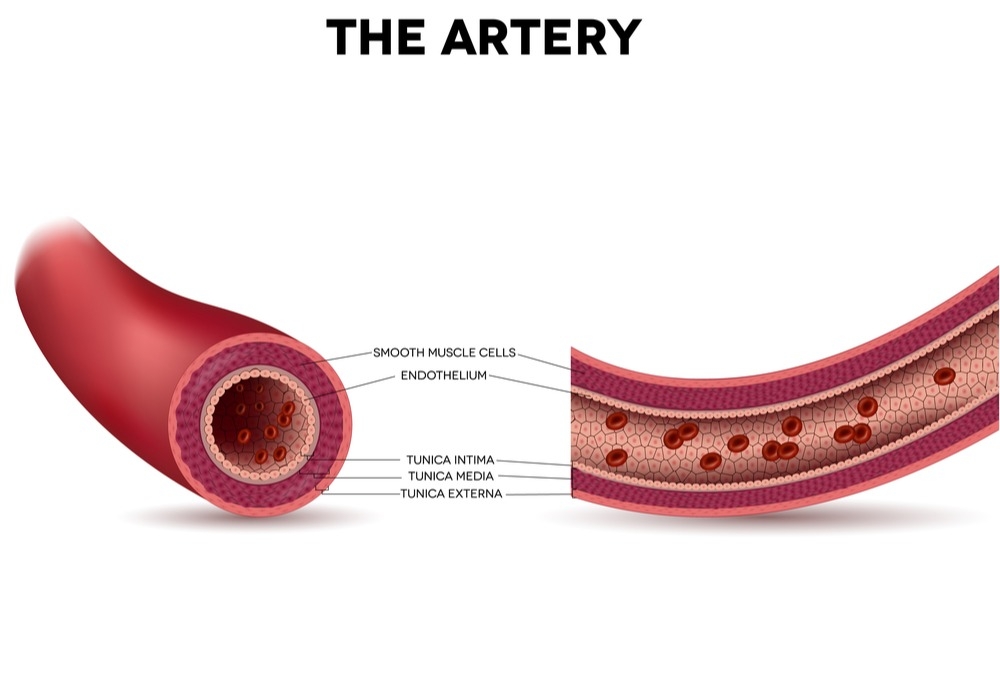
Instead of opening the chest, abdomen, or limbs for direct access to the arteries, these methods rely on accessing the vascular system through a very small incision, typically in the groin or wrist area.
A thin, flexible tube called a catheter is inserted, and guided by advanced imaging techniques such as fluoroscopy or 3D imaging, the catheter is pushed through the blood vessels to reach the affected area.
This catheter allows precise and specialized tools to be delivered inside the artery to treat the problem.
These techniques began to develop in the late 1980s and early 1990s, and have seen tremendous leaps in precision, safety, and effectiveness due to improved materials (such as adaptive Nitinol alloys) and the development of miniature tools.
The primary goal is to restore normal blood flow or prevent rupture of dilated blood vessels, all with the least possible surgical intervention.
This continuous development makes them an increasingly important option for patients who may not be eligible for open surgery due to health risk factors.
Types of “Closed” Artery Replacement Procedures
Although the term “replacement” might suggest complete removal and implantation of a new artery, closed techniques focus on rebuilding or supporting the artery from within.
Specializing in these procedures requires high expertise, and Liva Hospital in Turkey is one of the centers that offers these advanced procedures. Among the most prominent of these procedures are:
- Angioplasty and Stenting:
- Mechanism: This technique is used to treat narrowed or blocked arteries (especially in the legs, kidneys, or carotid arteries).
A catheter carrying a small balloon is inserted into the narrowed artery, and the balloon is inflated to open the artery.
Afterward, a stent, which is a small metal mesh tube, is often placed inside the artery to keep it open and prevent re-narrowing.
There are different types of stents, including drug-eluting stents that release medication to prevent cellular regrowth that might cause new narrowing. - Application: Widely used in Peripheral Artery Disease (PAD) to relieve claudication and improve wound healing, in the carotid artery to prevent stroke (Carotid Stenting), and in renal arteries to treat high blood pressure.
- Mechanism: This technique is used to treat narrowed or blocked arteries (especially in the legs, kidneys, or carotid arteries).
- Endovascular Aneurysm Repair (EVAR / TEVAR):
- Mechanism: This technique is a significant alternative to open surgery for repairing aortic aneurysms in the abdomen (EVAR) or chest (TEVAR).
Instead of replacing the dilated part of the artery, a stent-graft, which is a mesh tube covered with synthetic fabric, is inserted via a catheter and deployed inside the dilated aorta.
This stent-graft acts as a new internal conduit for blood, preventing blood pressure from pressing on the aneurysm wall and reducing the risk of rupture. - Application: This technique is preferred for patients considered high-risk for open surgery, or those with an aneurysm of suitable shape and size for stent placement.
- Mechanism: This technique is a significant alternative to open surgery for repairing aortic aneurysms in the abdomen (EVAR) or chest (TEVAR).
Advantages of the “Closed Approach” Compared to Open Surgery
Endovascular techniques (the closed approach) offer numerous fundamental advantages compared to traditional open surgery, making them the preferred choice for many patients:
- Less Invasive: The procedure is performed through very small incisions (usually a few millimeters), which means less damage to surrounding tissues and avoids the need for a large incision and opening chest or abdominal bones.
- Less Post-Surgical Pain: Due to reduced surgical trauma, patients experience significantly lower levels of pain after the operation, reducing the need for strong pain relievers.
- Shorter Recovery Time: Patients can return home within a day or two after most catheter procedures, compared to a week or more for open surgery. Return to daily activities and work is also much faster.
- Lower Risk of Complications: Generally, these techniques are associated with lower risks of infection, severe bleeding, and large scars.
- Suitable for High-Risk Patients: Due to their less invasive nature, these procedures are a vital option for elderly patients or those with chronic health conditions (such as severe heart or lung disease) that make them ineligible for open surgery.
- Better Cosmetic Results: They leave very small and almost invisible scars, which many prefer aesthetically.
Preparing for Surgery and Post-Operative Care
Despite their less invasive nature, closed-approach artery replacement procedures require careful preparation and effective post-operative care to ensure the best outcomes.
- Pre-Surgical Preparation: This includes a comprehensive evaluation of the patient’s condition, including a review of medical history, physical examination, and detailed imaging tests (such as Computed Tomography Angiography – CTA).
The patient may be asked to stop certain medications, such as blood thinners, for a short period before the operation. Instructions are provided regarding fasting and preparing the patient for the procedure. - During the Procedure: Most of these procedures are performed under local anesthesia with intravenous sedation, allowing the patient to remain awake but relaxed. The patient’s vital signs are continuously monitored.
- Immediate Post-Surgical Period: After the procedure, the patient is transferred to the recovery room for observation for a few hours.
They may be asked to lie flat for several hours to ensure the catheter insertion site closes properly. - Recovery in Hospital and at Home: The patient can return home on the same day or after one night in the hospital, depending on the type of procedure and their health condition.
The doctor provides instructions on wound care, medications to take (especially antiplatelet drugs for some time), and when normal activities can be resumed. - Regular Follow-up: Regular follow-up with the doctor is essential to assess the success of the procedure, monitor the graft or stent, and manage risk factors that may cause future problems. Follow-up may include Ultrasound Duplex Scans or CT Scans.
Who is the Closed Approach Suitable For?
Reliable studies and medical sources indicate that the effectiveness of these procedures is very high in carefully selected cases.
Although some complex cases may still require open surgery, the closed approach offers a safe and effective alternative for most patients, with continuously improving long-term results thanks to ongoing innovation in medical technology.
The applications of closed-approach artery replacement have expanded to include a wide range of conditions, making it an attractive option for many patients. These techniques are particularly suitable for cases involving:
- Narrowing and Blockages of Peripheral Arteries (PAD): Especially in leg arteries, where they help relieve pain, improve blood flow, and save limbs from amputation.
- Carotid Artery Disease: Treatment of carotid artery narrowings (Carotid Stenting) as an alternative to endarterectomy in some cases, especially for high-surgical-risk patients.
- Aortic Aneurysm: Endovascular repair of abdominal or thoracic aortic aneurysms (EVAR/TEVAR) is a standard option for many patients, and is now often preferred over open surgery due to its advantages.
- Renal Artery Stenosis: Using catheters and stents to improve blood flow to the kidneys, which may help control high blood pressure or improve kidney function.

Challenges in Artery Treatment
Despite significant progress, endovascular techniques still face challenges.
Not all cases are suitable for treatment with the closed approach, especially when narrowings are very long, heavily calcified, or when aneurysms have complex anatomy unsuitable for covered stents.
Additionally, some stents may experience “re-narrowing” in the long term, requiring additional interventions.
However, the future looks very promising. Research and development focus on:
- Improving Stent Design and Materials: To be more flexible, longer-lasting, and less prone to re-narrowing.
- Developing New Tools: Enabling access to and effective treatment of more complex arteries.
- Hybrid Procedures: Combining limited open surgery and catheter procedures simultaneously to treat highly complex cases.
- Artificial Intelligence and Advanced Imaging: To improve diagnostic accuracy and guide procedures.
Conclusion
“Replacing” arteries with the closed approach is not just a technological advancement; it is a fundamental shift in how we approach vascular diseases.
These techniques have changed the lives of thousands of patients, offering them a less painful and faster-recovering treatment option, with excellent clinical outcomes.
Through tiny incisions and precise catheters, doctors today can repair and restore damaged arteries, restore blood flow, preserve limbs, prevent strokes, and save lives.
This revolution in endovascular treatment represents a milestone in modern medicine, bringing hope for a healthy and active life to a larger number of individuals.
Liva Hospital in Turkey is one of the advanced institutions in this field, with distinguished experts and technologies, striving to provide the best options for each patient according to their unique condition.
Frequently Asked Questions
How long does it take to return home after a closed-approach procedure?
In most cases, patients can return home on the same day or after only one night in the hospital, depending on the type of procedure and their health condition.
Do closed-approach procedures leave large scars?
No, these procedures are performed through very small incisions (a few millimeters), meaning they leave very small and almost invisible scars compared to the large scars of open surgery.
Can I drive after closed-approach artery replacement?
Generally, most patients can resume driving within a few days to a week after most catheter procedures, but you should always consult your doctor for specific instructions for your situation.
Do I need to take medications after closed-approach artery replacement?
Yes, in most cases, your doctor will prescribe antiplatelet medications (such as aspirin or clopidogrel) to prevent blood clots from forming on the stent or within the blood vessels, and these medications are usually taken for a long time or lifelong.
What is the success rate of these procedures?
The success rate of closed-approach artery replacement procedures is very high, exceeding 90% in many cases, especially when performed in specialized centers.
Can the problem recur after closed-approach treatment?
Yes, although grafts and stents are designed to last, there is a small chance of re-narrowing or new problems occurring in the future.