Your heart beats in harmony. Its internal chambers synchronize to keep you alive and healthy.
Unfortunately, not everyone is so lucky. Some heart failure patients suffer from a defect called ventricular dyssynchrony.
Here, the contractions of the left and right ventricles are uneven. This worsens the heart’s pumping efficiency.
Also, Coronary Artery Disease (CAD) is a leading cause of death and disability worldwide.
Fatty plaques accumulate inside the arteries that supply the heart muscle. This leads to their narrowing. It reduces blood and oxygen flow to the heart.
This is where Cardiac Resynchronization Therapy (CRT), or heart stent technology, plays a pivotal role. Electrical leads and tiny devices are implanted to restore harmony and increase pumping efficiency.
This method is considered an advanced technique. It’s available in centers like Liva Hospital in Turkey. It’s applied with the latest standards and practices to ensure the best outcomes for patients.
Coronary Artery Disease
Coronary Artery Disease (CAD) is a condition that affects the coronary arteries. These are the blood vessels that supply oxygen-rich blood to the heart muscle. This disease usually occurs due to atherosclerosis.
This is a process where fatty plaques (cholesterol, fats, calcium, and other substances) accumulate inside the artery walls.
This causes them to narrow and harden. This narrowing hinders sufficient blood flow to the heart muscle. Especially during physical exertion or emotional stress.
Symptoms of CAD can develop gradually or appear suddenly:
- Angina (chest pain)
- Shortness of breath
- Extreme fatigue
- Heart attack
Indications for Heart Stent Implantation
Heart stent implantation, also known as coronary angioplasty with stents, is a primary treatment option for CAD patients. Especially in cases that can’t be controlled with medication alone.
Or in emergency situations like heart attacks. The main indications for heart stent implantation include:
- Relief of Angina Symptoms: When angina is frequent or severe. It affects the patient’s quality of life. And it doesn’t respond to medication.
- Opening Blocked or Narrowed Arteries: Restoring normal blood flow to the heart muscle.
- Managing Heart Attacks (STEMI/NSTEMI): In cases of acute heart attack, the procedure is performed urgently. This is to open the blocked artery as quickly as possible. It reduces heart muscle damage.
- Improving Outcomes of Medical Treatment: When diagnostic tests (like cardiac catheterization) indicate significant narrowing in the coronary arteries.
- Prevention of Future Heart Attacks: By improving blood flow and reducing the heart’s workload.
Types of Heart Stents Used
Heart stents have undergone significant development since their first appearance.
This has led to major improvements in patient outcomes and reduced complications. Heart stents are primarily classified into two types:
Bare-Metal Stents (BMS)
These stents are made from metal alloys (such as stainless steel or cobalt-chromium).
Their primary function is to provide structural support to the artery after balloon expansion. This prevents it from re-collapsing.These were the first generation widely used.
However, a common problem was In-Stent Restenosis. This occurs when cells grow excessively inside the stent. It causes a new narrowing of the artery. The restenosis rate is estimated at 20-30% with bare-metal stents.
Drug-Eluting Stents (DES)
These stents are the gold standard in modern times. They consist of a metal stent coated with a thin polymer layer.
This slowly releases a specific drug (usually cell proliferation inhibitors) over weeks or months. This drug aims to prevent excessive cell growth inside the stent. This significantly reduces restenosis rates (to about 5-10% or less).
Despite their high effectiveness, DES require a longer period of dual antiplatelet therapy (such as aspirin and clopidogrel). This reduces the risk of Stent Thrombosis, a rare but serious complication.
Preparing for Heart Stent Implantation
Good and prior preparation for heart stent implantation is crucial. It ensures patient safety. And it achieves the best possible outcomes.
This preparation usually begins a few days before the procedure date. It includes a comprehensive set of medical examinations and preventive instructions.
- Comprehensive Medical Evaluation: The cardiologist and nursing team will perform a series of medical examinations. This assesses the patient’s general health. And their suitability for the procedure.
- Medication Discussion: The patient will be asked to provide the doctor with a complete list of all medications they are taking. This includes nutritional supplements and herbs.
- Antiplatelet Therapy: The patient is often prescribed an antiplatelet drug (such as aspirin and clopidogrel or ticagrelor). They start taking it a day or two before the procedure. This medication is essential. It reduces the risk of clot formation inside the stent after implantation.
- Fasting: The patient must refrain from food and drink for a certain number of hours (usually 6-8 hours) before the procedure. This is according to the doctor’s instructions. It ensures the safety of the local or light anesthesia used.
- Removal of Personal Items: The patient will be asked to remove any jewelry, glasses, contact lenses, dentures, or hearing aids before the procedure.
- Education and Informed Consent: Fully understanding the procedure is vital. This includes potential risks and benefits. And what to expect during and after the operation.
The doctor will explain the procedure in detail. They will answer all patient questions. The patient will be asked to sign an informed consent form. - Planning for Post-Procedure: Although the patient may go home the same day or the next, it is advisable to arrange for someone to drive them home. Driving is not allowed immediately after the procedure.
What Happens During Heart Stent Implantation?
Heart stent implantation is a procedure that requires high precision and extensive experience.
The procedure is performed in a Cardiac Catheterization Lab (Cath Lab). It usually takes about one to two hours. But it may take longer in complex cases.
- Access and Blood Vessels:
- The patient is given a light sedative to help them relax. Local anesthesia is applied to numb the access site.
- The interventional cardiologist chooses the access site. This is often the femoral artery in the groin area. Or the radial artery in the wrist. The radial artery is currently preferred more and more. This is to reduce the risk of bleeding and complications at the access site.
- The doctor makes a small incision in the skin. They insert a protective sheath into the artery. This is used as a safe entry point for instruments.
- Catheter Insertion and Access to the Heart:
- The doctor inserts a thin, flexible guidewire through the protective sheath. They carefully guide it through the major arteries. This reaches the coronary arteries that supply the heart.
This guidance is assisted by continuous Fluoroscopy (X-ray images) displayed on screens in the cath lab.
- After the guidewire reaches the affected coronary artery, a larger guiding catheter is passed over the wire. It is positioned at the opening of the coronary artery.
- The doctor inserts a thin, flexible guidewire through the protective sheath. They carefully guide it through the major arteries. This reaches the coronary arteries that supply the heart.
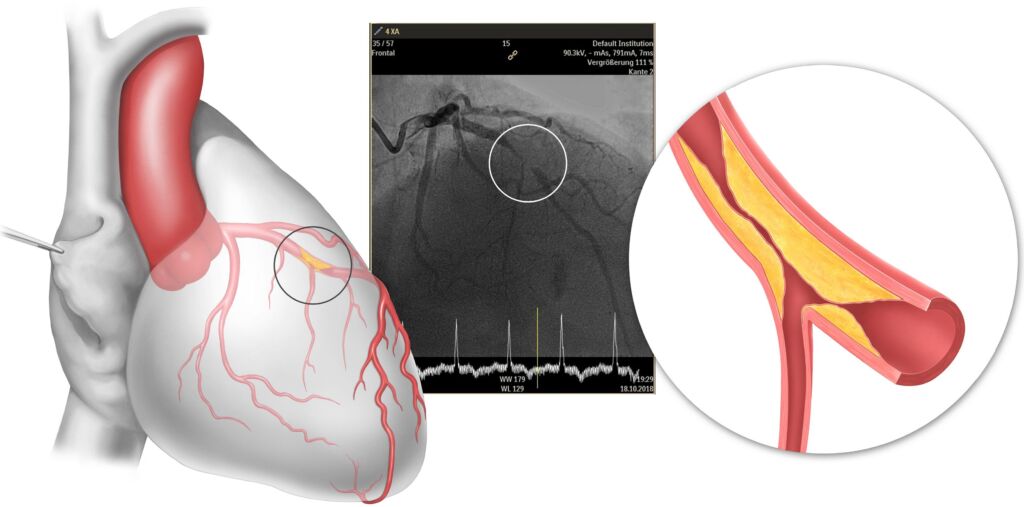
- Angiography (Artery Imaging):
- A special dye (contrast material) is injected through the guiding catheter into the coronary arteries. This dye clearly shows the arteries on X-ray images.
This allows the doctor to accurately see the narrowings or blockages. And to determine their location, size, and severity.
- A special dye (contrast material) is injected through the guiding catheter into the coronary arteries. This dye clearly shows the arteries on X-ray images.
- Balloon Angioplasty (Artery Widening):
- A very thin balloon catheter is passed over the guidewire. It is positioned inside the narrowed artery.
- The balloon is inflated for several seconds. This presses the fatty plaques against the artery walls. It widens the artery and restores blood flow. The balloon may be inflated several times.
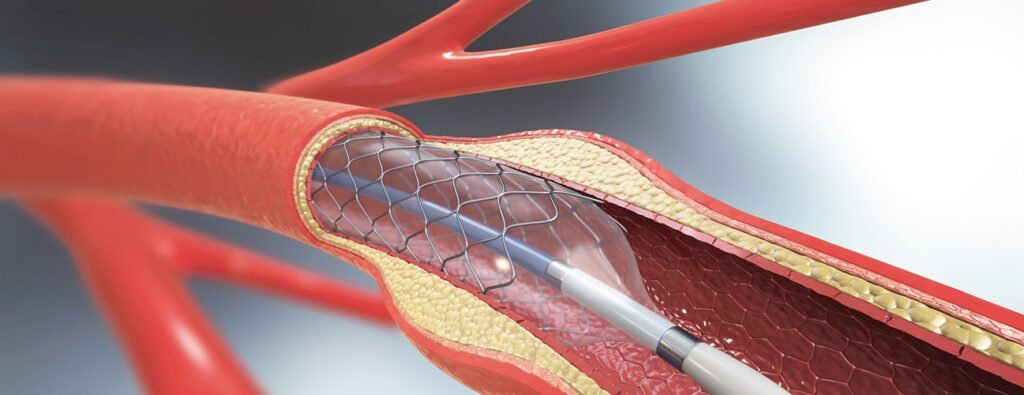
- Stent Implantation:
- After balloon widening, the heart stent (which is mounted around another balloon) is passed into the narrowed artery.
- The balloon holding the stent is inflated. This opens the stent and makes it adhere to the artery wall. The stent forms a permanent scaffold that keeps the artery open.
- The balloon is deflated and carefully withdrawn, leaving the stent in place.
- Verifying Results and Closing the Access Site:
- The dye is re-injected. This ensures the stent is correctly positioned. And that blood flow has effectively improved.
- The catheter and guidewire are withdrawn. The access site in the groin or wrist is closed. This is done using manual pressure techniques or special closure devices. This ensures bleeding stops.
Recovery After Heart Stent Implantation
The recovery period after heart stent implantation is much faster and less complicated compared to open-heart surgery.
Most patients can return home the same day or the day after the procedure.
- Early Stage (In Hospital – Hours to One Day):
- Monitoring: After the procedure, the patient is transferred to a monitoring room. Here, vital signs (blood pressure, pulse, breathing) and the access site are monitored for any bleeding or swelling.
- Rest: The patient is asked to rest in bed for several hours. Especially if the access site was in the groin. This is to avoid bleeding.
- Pain Management: Pain is usually mild. It can be controlled with over-the-counter pain relievers.
- Fluids and Food: The patient can start taking fluids and light food as soon as their condition allows.
- Hospital Discharge: In most cases, the patient can be discharged from the hospital on the same day or the morning of the next day. This is once their condition is stable. And they are able to walk.
- Intermediate Stage (At Home – Days to Weeks):
- Access Site Care: The patient must keep the access site clean and dry. There might be a small bruise or mild swelling, which gradually disappears.
- Physical Activity: It is recommended to start walking short distances. And to gradually increase activity. Heavy lifting or strenuous physical activities should be avoided for several days to a week.
- Medications: Adherence to prescribed medications is crucial. Especially antiplatelet drugs (aspirin and another drug like clopidogrel or ticagrelor). These medications prevent clot formation inside the stent. They also reduce the risk of its blockage.
The duration of taking these medications may last for several months or years. This depends on the type of stent and the patient’s condition.
- Nutrition and Lifestyle: It is recommended to follow a heart-healthy diet. Quit smoking (if applicable). Maintain a healthy weight. And exercise regularly.
- Cardiac Rehabilitation Programs: Joining a Cardiac Rehabilitation program may be recommended. This is a supervised program. It helps patients regain their strength. It also teaches them how to manage heart disease. And how to improve their lifestyle.
- Long-Term Stage (Months and Years):
- Regular Follow-up: Regular follow-up with a cardiologist is essential. This assesses cardiac health. It also monitors medication effectiveness. And it performs necessary examinations.
- Adherence to a Healthy Lifestyle: Maintaining a healthy lifestyle is vital in the long term. This prevents the development of more coronary artery narrowing in other areas.
These procedures do not treat the underlying disease of atherosclerosis. But they improve blood flow.
Potential Risks and Complications
Although heart stent implantation is considered safe and effective, like any medical procedure, it carries some potential risks and complications.
These complications are relatively rare. But it’s important for patients to be aware of them. And to discuss them with their doctor.
- Risks Associated with the Access Site (Groin or Wrist):
- Bleeding or bruising: The most common, usually mild. In rare cases, bleeding may be severe and require intervention.
- Hematoma formation: A collection of blood under the skin.
- Infection: At the access site, which is rare.
- Artery damage: Rarely, a puncture in the artery or damage to the surrounding nerves.
- Risks Associated with the Heart and Coronary Arteries:
- Heart attack: A heart attack can occur during or after the procedure. Especially if there is a sudden blockage of the treated artery. Or if a blood clot forms.
- Stroke: Although very rare, stroke can occur due to a blood clot or plaque traveling to the brain.
- Coronary Artery Dissection/Perforation: A tear or puncture in the coronary artery wall may occur. This is a serious complication. It may require emergency open-heart surgery.
- Arrhythmias: May occur during the procedure. Usually temporary.
- Allergic reactions: To the contrast dye used in X-rays or other medications.
- Kidney problems: The contrast dye used in X-rays can cause temporary or permanent kidney damage. Especially in patients with pre-existing kidney problems.
- Stent Thrombosis: A rare but serious complication. It occurs when a blood clot forms inside the stent after implantation. This leads to artery blockage. Dual antiplatelet therapy significantly reduces this risk.
- In-Stent Restenosis: Although drug-eluting stents have significantly reduced this risk, it is still possible. It occurs when cells grow excessively inside the stent. This causes new narrowing. This may require an additional procedure.
Outlook and Outcomes After Heart Stent Implantation
Heart stent implantation is a highly effective procedure. It improves symptoms. It reduces the risk of heart attacks.
And it enhances the quality of life for patients with coronary artery disease. Long-term outcomes largely depend on several factors:
- Symptom Improvement: The majority of patients report significant improvement in angina and shortness of breath symptoms after stent implantation. This allows them to resume daily activities more comfortably.
- Reduced Risk of Heart Attacks: By restoring normal blood flow, stents reduce the risk of future heart attacks related to the treated artery.
- Success Rates: Studies show that coronary angioplasty with stent implantation has high success rates in opening narrowed arteries. This exceeds 90% in most cases.
- Quality of Life: The procedure significantly contributes to improving the patient’s quality of life. This enables them to return to a more active and independent lifestyle.
- Need for Additional Treatments: In some cases, additional procedures may be needed in the future. This is if new narrowing develops in other arteries. Or if in-stent restenosis occurs.
- Importance of Lifestyle and Medications: Adherence to prescribed medications (especially antiplatelet drugs). And lifestyle modifications (like quitting smoking, following a healthy diet, and exercising).
All are crucial for maintaining the procedure’s results. And for preventing future heart problems. These procedures do not treat the underlying disease of atherosclerosis. But they improve blood flow.
Conclusion
Heart stent implantation (CRT) represents a therapeutic breakthrough. It’s for heart failure with ventricular dyssynchrony.
Its success is based on careful patient selection, professional technique, and the importance of serious follow-up.
Thanks to continuous developments in stent design and procedural techniques, the procedure has become safer and more effective than ever before.
However, it’s essential to emphasize that stent implantation is not a magic solution that eliminates the need for a healthy lifestyle.
Adherence to a balanced diet, regular physical activity, quitting smoking, and consistently taking prescribed medications are all vital elements.
They help maintain heart health after the operation. And they prevent future problems.
Liva Hospital in Turkey stands out as an advanced center. It utilizes high technologies and precise follow-up programs. This enhances patients’ chances for significant improvement and a better quality of life.
Frequently Asked Questions
Is heart stent implantation painful?
No, the procedure is performed under local anesthesia at the access site (groin or wrist). You may also be given a sedative to help you relax. Therefore, you won’t feel pain during the procedure itself. You might feel some mild pressure or discomfort at the access site after the procedure.
How long does stent implantation take?
The procedure usually takes about one to two hours. However, the duration may vary depending on the number of arteries to be treated and the complexity of the case.
When can I return to normal activities after stent implantation?
Most patients can return to light daily activities (like light walking) within a day or two after the procedure. It’s advised to avoid heavy lifting or strenuous physical activities for several days to a week. Your doctor will provide you with detailed instructions based on your condition.
Will I need to take medications for life after stent implantation?
Yes, you will need to take some medications for life, especially aspirin. Other antiplatelet medications (like clopidogrel or ticagrelor) are usually prescribed for 6 months to a year or more, depending on the type of stent and your condition. These medications are essential to prevent clot formation inside the stent.
What are the chances of artery re-blockage after stent implantation?
Drug-eluting stents (DES) have significantly reduced the risk of in-stent restenosis to about 5-10% or less. However, it is still possible. Adherence to medications and a healthy lifestyle greatly reduces this risk.
Can a heart stent move inside the artery?
No, once the stent is opened inside the artery and adheres to its walls, it integrates with the artery wall over time and becomes a permanent part of it. It’s very rare for a stent to move from its place after being correctly implanted.