We are in an era where new medical technologies are constantly emerging.
They are changing treatment concepts. And they offer hope for patients suffering from heart problems.
Medication used to be the first choice for controlling heart rhythm disorders. But it often comes with side effects. Or it might not provide enough control.
However, thanks to advances in cardiac electrophysiology, Cryoablation has emerged as an innovative and effective alternative.
It offers a unique approach to correcting these heart rhythm disorders. Unlike traditional thermal ablation, cryoablation uses very low temperatures to destroy the cells responsible for faulty electrical signals.
This safely and precisely restores the heart’s natural rhythm.
This technique treats sources of abnormal electrical activity by freezing them. It doesn’t use heat.
This reduces the risk of collateral damage and increases safety. This technique is modern and advanced.
It is applied by advanced medical teams at Liva Hospital in Turkey. This is part of comprehensive programs for treating heart rhythm disorders.

Heart Rhythm Disorders and the Use of Cryoablation
The heart is the body’s vital pump. It functions thanks to a complex electrical system.
This system generates and transmits electrical signals with extreme precision. It coordinates heart muscle contractions.
When this electrical system malfunctions, heartbeats become irregular. They can be too fast or too slow. This is known as Arrhythmias.
Among the types of arrhythmias, some are more common and treatable with cryoablation:
- Atrial Fibrillation (AFib): Atrial fibrillation is the most common. Here, the atria (the heart’s upper chambers) beat rapidly and irregularly.
This hinders efficient blood flow. It also increases the risk of blood clots. And therefore, the risk of stroke. Atrial fibrillation can cause symptoms like palpitations, shortness of breath, fatigue, and dizziness. - Atrial Flutter: This is another type of supraventricular tachycardia. Here, electrical signals in the atria are rapid and relatively regular. This leads to fast and regular heartbeats.
- Supraventricular Tachycardia (SVT): This is a general term for various types of rhythm disorders. They start in the atria or the atrioventricular node. They cause rapid heartbeats. These include Wolff-Parkinson-White syndrome (WPW) and other types.
Principles of Cryoablation
Unlike Radiofrequency Ablation, which uses heat to destroy cells causing rhythm disorders, Cryoablation relies on using extreme cold to achieve the same goal. This approach is revolutionary. It offers unique advantages. And it reduces some of the potential risks of thermal ablation.
- Extreme Cold for Cell Destruction:
- A special catheter is used. It releases an extremely cold cryo-agent (like nitrous oxide) from its tip. When the catheter tip touches the targeted heart tissue, the tissue’s temperature rapidly drops below zero (usually ranging from -70 to -80 degrees Celsius).
- This extreme cold causes ice crystals to form inside the cells. This destroys vital cellular structures. And it leads to the death of cells responsible for generating or transmitting abnormal electrical signals.
- This destruction forms a small scar area (cryolesion). This electrically isolates the area causing the arrhythmia.
- “Freeze Test” Advantage:
- One of the most notable advantages of cryoablation is the ability to perform a “Cryo-mapping” or “freeze test” before permanent tissue destruction.
- When a slightly lower temperature is applied (around -20 to -30 degrees Celsius), the tissue is temporarily frozen. If the arrhythmia disappears during this “temporary freeze,” it indicates that the targeted area is indeed the source of the problem.
- If any complications or undesirable side effects are observed during this test (such as affecting nearby sensitive normal electrical pathways), the cold can be removed. This allows the tissue to return to its normal function without permanent damage. This feature significantly reduces the risk of serious complications, such as damage to the AV Node or the Phrenic Nerve.
- More Consistent Scar Formation:
- Cryoablation is believed to produce more homogeneous and consistent scars compared to thermal ablation. This may contribute to achieving better long-term results in some cases.
What Happens During a Cryoablation Procedure?
Cryoablation is a highly precise procedure. It is performed in a specialized electrophysiology lab. It usually takes 2 to 4 hours.
In specialized hospitals like Liva Hospital in Turkey, the latest protocols and techniques are applied. This ensures the highest levels of precision and safety for patients undergoing this procedure.
- Anesthesia and Access:
- The patient receives appropriate anesthesia. Local anesthesia at the access site (groin) with intravenous sedation is often used to help the patient relax. In some cases, especially for atrial fibrillation, general anesthesia may be preferred.
- The doctor makes a small incision (usually in the groin area). They insert several sheaths into the femoral veins (and sometimes arteries). These sheaths are used as safe pathways for inserting catheters.
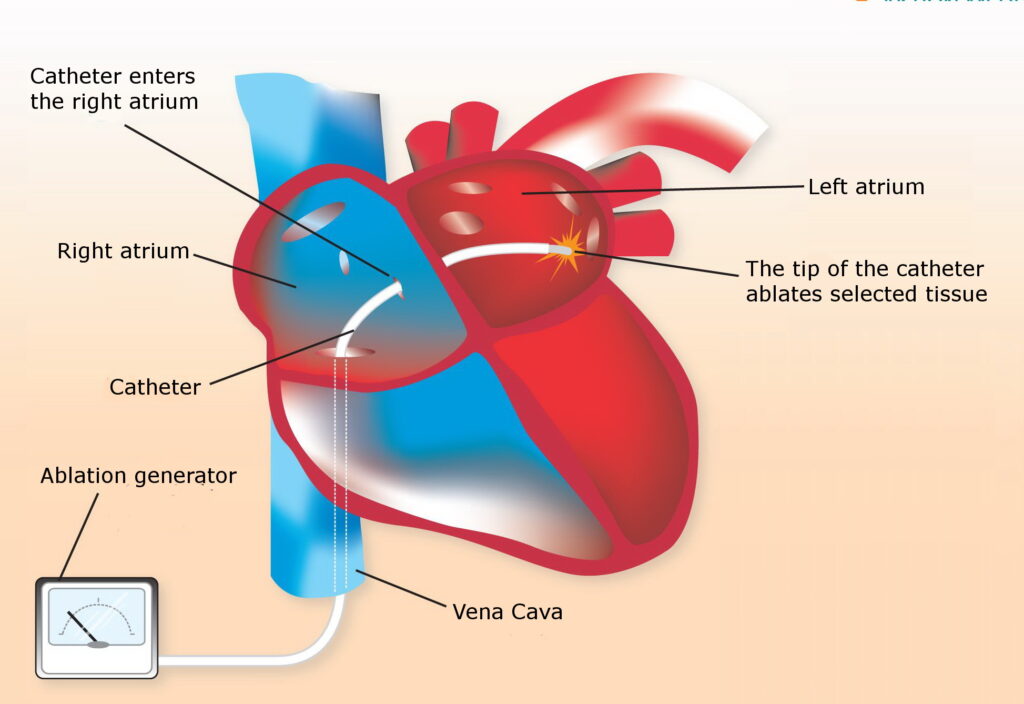
- Guiding Catheters to the Heart:
- Thin, flexible catheters (Cryoablation Catheter and a set of mapping catheters) are inserted through the sheaths. They are carefully guided through the blood vessels to different heart chambers (usually the left atrium in cases of atrial fibrillation).
- This guidance is assisted by real-time Fluoroscopy (X-ray images) and advanced 3D Mapping Systems like CARTO or EnSite Precision. These systems provide a detailed map of the patient’s heart and precisely locate the catheters and areas of abnormal electrical signals.
- Identifying the Source of Arrhythmia (Mapping):
- Using mapping catheters, the doctor identifies the abnormal electrical pathways or foci that are emitting irregular electrical signals.
- In atrial fibrillation, the focus is often on isolating the pulmonary veins. These are common areas that emit abnormal electrical signals causing the arrhythmia.
- Applying Cryoablation:
- Once the target area is precisely identified, the cryoablation catheter is guided to this location.
- The cryo-gas is released from the catheter tip. This causes a rapid drop in temperature and freezes the tissue.
- The doctor carefully monitors the effect of the freezing. This includes the possibility of a “freeze test” (as mentioned earlier) to ensure effectiveness and safety.
This process is repeated several times. The goal is to create lines of ablation that electrically isolate the problematic areas.
- During pulmonary vein freezing, the Phrenic Nerve is carefully monitored to avoid damage. This nerve controls the movement of the diaphragm (the main muscle for breathing).
- Verifying Success and Removing Instruments:
- After ablation is complete, the doctor re-evaluates the heart’s electrical system. This ensures that the abnormal pathways have been successfully severed. And that the arrhythmia can no longer be induced.
- All catheters and sheaths are carefully withdrawn.
- The access site in the groin is closed with manual pressure or using special closure devices. This ensures bleeding stops.
Potential Risks and Complications of Cryoablation
Although cryoablation is generally considered a safe and effective procedure, like any medical intervention, it carries some potential risks and complications.
These complications are relatively rare, but it’s important for patients to be aware of them and discuss them with their doctor.
- Risks Associated with the Access Site (Groin):
- Bleeding or bruising: The most common, usually mild. In rare cases, bleeding may be severe and require medical intervention.
- Hematoma formation: Blood collection under the skin.
- Infection: At the access site, very rare.
- Blood vessel damage: Rarely, a puncture or tear in the femoral vein or artery.
- Risks Associated with the Heart and Procedure:
- Pericardial Effusion/Tamponade: A serious but very rare complication (less than 1%). It occurs if the heart wall is accidentally punctured by the catheter. This leads to fluid accumulation around the heart and pressure on it. It may require fluid drainage or emergency surgery.
- Phrenic Nerve Injury: This risk is more specific to cryoablation, especially when isolating the right upper pulmonary veins. The phrenic nerve controls the movement of the diaphragm (the main muscle for breathing).
Damage to this nerve may cause temporary or permanent weakness of the diaphragm, which can lead to shortness of breath. However, this complication is rare (less than 3%).
In most cases, it is temporary and improves over time. Special monitoring techniques are used during the procedure to reduce this risk. - Blood Clots and Stroke: Although rare, a blood clot may form on the catheter tip or in the heart. It can then travel to the brain (causing a stroke) or to other parts of the body.
Blood thinners are used during and after the procedure to significantly reduce this risk. - Damage to the Normal Electrical Conduction System: The ablation process may affect the AV Node or other pathways. This causes slow heartbeats. It may require permanent pacemaker implantation.
Especially if the treated area is close to these vital structures. This risk is less common with cryoablation compared to thermal ablation near these areas. - Pulmonary Vein Stenosis: Rarely, narrowing of the pulmonary veins occurs after their isolation. This can cause shortness of breath.
- Atrioesophageal Fistula: An extremely rare and dangerous complication. Here, ablation creates a hole between the left atrium and the esophagus. Cryoablation reduces this risk compared to thermal ablation.
- General Risks:
- Radiation Exposure: From the X-rays used for guidance. Although the dose is relatively low, it is taken into consideration.
- Allergic Reactions: To anesthesia medications or dyes.
Conclusion
Cryoablation is a game-changer in the treatment of heart rhythm disorders. It offers new hope for millions suffering from irregular heartbeats.
By using extreme cold to freeze and destroy the abnormal cells responsible for these disorders, this technique provides superior precision.
It carries a lower risk to surrounding sensitive structures. And it has the unique “freeze test” advantage that enhances the safety of the procedure.
From atrial fibrillation to types of supraventricular tachycardia, this innovative technique enables patients to restore a normal heart rhythm.
This reduces debilitating symptoms. And it significantly improves their quality of life.
The extreme precision of cryoablation, combined with the comprehensive care provided by specialized centers like Liva Hospital in Turkey, enhances its position as a preferred treatment option.
Frequently Asked Questions
What is the main difference between cryoablation and radiofrequency ablation?
The main difference lies in the method of cell destruction. Radiofrequency ablation uses heat to burn and destroy the cells causing the arrhythmia, while cryoablation uses extreme cold to freeze and destroy those cells.
Is cryoablation painful?
No, the procedure is usually performed under local anesthesia at the access site (groin) with intravenous sedation to help you relax.
How long does the recovery period take after cryoablation?
Recovery after cryoablation is much faster than open surgery. Most patients can return home the same day or the day after the procedure. Light daily activities can be resumed within a few days.
Can arrhythmias return after cryoablation?
Although cryoablation is very effective, there is a small possibility of the arrhythmia returning over time. This risk is estimated at 15-30% in the case of atrial fibrillation after the first session.
Do I need to take blood thinners after the procedure?
If you suffer from atrial fibrillation, you will often need to continue taking blood thinners (like warfarin or novel oral anticoagulants) to prevent clots.
What are the most common complications with cryoablation?
The most common complications are related to the access site (such as bleeding or bruising). More serious but very rare complications include phrenic nerve damage (which controls the diaphragm) or heart perforation.